A Model for Return to Training and Competition During Ongoing Pandemic Concerns
Michael R. P. de la Roche1, David M. Telles-Langdon2*, and Marc Robin
1Department of Family Medicine, Queen’s
University
2Kinesiology and Applied Health, University of Winnipeg
Submitted April 2022 | Accepted in final form June 2022
de la Roche et al. In the wake of a novel Coronavirus, the sports world reeled from the realization that a pandemic of this magnitude had not been seen in more than a century. Reducing the transmission would require physical distancing to such a degree that it would necessitate the suspension of all sporting activities. The multidimensional health effects due to COVID-19 will be far more severe and prolonged if athletes cannot engage in sport at all. Most coaches are concerned with strength and conditioning maintenance as well as technical skill development in response to changes in the sport. Bringing athletes together to train while adhering to government-mandated protective measures, such as facemask use and physical distancing, proved to be a herculean task. The challenge for all sports is how to train in the setting of the new physical distancing required for a healthy community. Sail Canada ran a nine-day training camp and regatta utilizing the knowledge of a team of medical experts to adhere to the government-mandated restrictions without significantly compromising the athletic preparation. The event was a great success and could stand as a model for other sports to maintain training while still protecting the health and wellness of athletes, coaches, and officials.
Key Words: COVID-19, pandemic, coaching, training
The novel coronavirus SARS-CoV-2, which causes the COVID-19 infection, has had a profound effect on all aspects of society worldwide, including sporting events and training. The requirement for physical distancing and mask wearing has rendered athletes in many sports isolated from their ability to train and compete. With myriad competitive and training events having to be cancelled, and facilities being closed due to the global pandemic, coaches were forced to develop creative ways to provide athletes with training opportunities while ensuring they remain healthy in anticipation of future international competition. The substantive matter of interest in this article was the effective operationalization of a sailing event, but the model could be applied to many other outdoor sports. This article was written from a Canadian perspective and so was bound by the local guidelines concerning COVID-19. It is our assumption that several of the strategies employed to control the spread of COVID-19 may have been successful since none of the participants tested positive for the virus up to two weeks following the event. However, the question remains how to continue essential training while adhering to these virus mitigation strategies for many sports.
In response to the government’s COVID-19 health restrictions and guidelines, Sail Canada’s (the organizing authority for sailing in Canada) coaching staff, recognizing the needs of elite level athletes, organized a training and competition event. Athletes from across Canada, along with the support of their respective coaches, came to train and compete together for the first time in more 15 months. This was as much a trial in how to safely coach in the setting of COVID-19 as it was a practical exercise to provide training and competition for Canada’s top sailing athletes. The nine-day event included four of the nine Olympic sailing events. Men’s and women’s singlehanded (Laser class for males and Laser Radial class for females) and doublehanded (49er skiff for males and 49erFX skiff females) events ran from August 21-29, 2020, before vaccination was available, such that all participants were therefore unvaccinated. As a pilot project this is more of a descriptive article and many of the protocols explained were designed as issues emerged.
The Contextual Advantage for Sailing
During a pandemic, many sports cannot function because the nature of the specific sport means general physical distancing from other competitors and coaches is not possible. This would include all contact and combative sports and many team sports (soccer, hockey, football, etc.), where there is an inability to control the proximity of one competitor to another, as well as artistic sports that require spotting (figure skating, gymnastics, etc.). Certainly, individual sports can train in isolation, or with a physically distanced coach. However, for many sports the competition must be adapted (staggered starts, etc.) to meet the public health requirements.
Unlike sports such as long-distance running or weightlifting, where training alone can maintain or even improve their performance, the ability to train in technical/tactical/strategic sports like sailing relies on comparison. It is essential to train and compete simultaneously with others to determine what techniques, strategies, and tactics lead to improved performance. Fortunately, within the context of COVID-19, sailing and the associated need for physical distancing is the very nature of the sport. Athletes in double-handed boats must function together in a social bubble (defined later). Also, each athlete must stay in their own boat, which is virtually always going to keep them greater than the 2-meter distance mandated by the safety margins for COVID-19 away from athletes in other boats and/or the coaches. As such, while on the water when either competing or training, the issue of proximity to another athlete or coach is a non-issue. The challenge is incorporating such measures when on land, rigging and de-rigging, as well as pre- and post-race or event debriefs with coaches.
Extensive COVID-19 mitigation strategies were put into place including an emergency action plan in the case that someone did begin to develop symptoms or test positive. No onsite testing was performed. This experience demonstrates that basic public health measures, when applied with consistency and rigor, can result in a safe environment for some sporting events. All participants (athletes, coaches, support staff) were required to sign daily attestation forms, have their temperatures checked, wear a mask, and physically distance while on shore in the boat park, and during launching and returning ashore.
Development of Protocols
To develop the protocols to be instituted a review of the current literature was conducted. Relevant databases related to respiratory disease were identified and searched using the following key words in various combinations: COVID-19, SARS-CoV-2, social/physical distance, mask use, mask compliance, and hand hygiene. Search engines, databases reviewed, and journals cited included the following:
Search Engine Used and Databases Reviewed
Following a rudimentary search using the Google Scholar search engine and its citation index, the following databases were used to secure the requisite articles. Ebscohost, Medline, Pubmed, Biomed Central, PsycInfo, and SPORTDiscus.
Journals Cited
The following journals were cited: Annals of the American Thoracic Society; Disease Modelling; International Journal of Environmental Research and Public Health; Journal of Infection; Infectious Disease Modelling; Infectious, Influenza and Other Respiratory Viruses; Journal of the American Medical Association; Nature Research Scientific Reports; and The Lancet.
Once a list of articles was produced, relevant articles were identified and retrieved from a university library online (including the use of inter-library loan). A reference list was also produced, which includes the article’s full citations. The results section will include a critique of selected articles that highlights key points and draws attention to possible limitations of the article.
Using the information collected and supplemented by information from medical personnel on the front line, a review of current protocols was developed.
1) Given that there is limited empirical data to support the efficacy of various disease mitigation practices, the publication process of peer-reviewed medical journals was used as the criterion for selecting various mitigation practices for review.
2) “Best practices” are examples of successful initiatives to limit the spread of COVID-19; there is no single best practice that universally meets the needs of all programs.
In addition to using this article, practitioners interested in using this as a model for running a similar event, are encouraged to review relevant articles listed in the reference list for further information.
Results of the Literature Review
Support for Mandating Mask-Use, Physical-Distancing, and Hand-Hygiene
The coaching staff, in conjunction with the medical personnel, identified three consistent priorities cited in the literature to help limit the spread of COVID-19. Physical-distancing, hand-hygiene, and mask-wearing were identified as the main measures (Chen, et al. 2020). Facemasks are one of a combination of measures, including physical distancing, hand washing, sufficient ventilation, and the avoidance of crowds and gatherings, that can reduce transmission of COVID-19 (Steinbrook, 2020). Physical distancing along with self-isolation are the most successful protocols to limit the spread of pathogens (Chen et al. 2020; Eikenberry et al. 2020) but these are impractical while trying to train a group of athletes when some level of contact is unavoidable.
Mask-use
Mask-use required the effective use of a mask. Masks are available in a variety of levels of filtering ability (Clapp et al., 2020; Fischer et al., 2020; Howard et al., 2020; Sickbert-Bennett et al., 2020). Cheng et al. (2020b) suggest that the use of facemasks provides a useful and low-cost adjunct to physical distancing and strong hand hygiene. Athletes, officials and administrators had to shift their focus from self-protection to altruism where facemask use becomes a symbol of solidarity in response to the pandemic.
Clark at al. (2020) described the unique challenge for coaches and to ensure adequate cooperation and compliance amongst participants. The athletes, officials, and administrators had to be persuaded of the importance of compliance. The medical team and the coaches highlighted their belief in the efficacy of healthy behaviors to promote compliance by modelling the health behavior recommendations. Although practicing health behavior recommendations is important within the current pandemic, it may also be useful as a starting point for developing appropriate health behaviors within the group for other public health concerns faced by athletes (e.g., annual flu season, long-distance travel, etc.).
Our observations contribute to the literature on the implementation of protocols calling for physical distancing, and face mask usage from a behavioral perspective. Specifically, we study the effect of masking on physical distancing with a combination of a field evaluation by medical experts and a complementing attestation (see Appendix B). An additional concern expressed by Seres et al. (2021) was to ensure that participants do not reduce other crucial precautions like physical distancing. The medical personnel determined that the most effective way to support adequate masking was to provide masks onsite on an as-needed basis. Although (K)N95 masks would have been the optimal choice, due to availability issues, American Society for Testing and Materials (ASTM) level 1 surgical masks were selected.
Physical Distancing
We prefer this term over “social distancing” because it clearly defines the parameters of the restriction rather than alluding to a limit on social interaction although that is curtailed to some extent by limiting handshaking, hugging, and kissing which are important greetings in many cultures. Physical distancing was eminently possible for all participants in this event and required no specific supplies. Chen et al. (2020) notes that keeping physically distant is problematic where children are involved. For children to consistently conform to new rules requires focused supervision and reinforcement. Fortunately, at this particular event children were not present, but many sports have significantly younger participants.
For the purposes of this study physical distancing was evaluated by observation. This was exacerbated by an inability for the observers to determine when athletes were in the same social bubble. Bubble identifiers in the form of a color coded garment of some sort would have aided in identifying failures in physical distancing.
Social Bubble. For the purposes of this event, it seemed prudent to define social bubbles and provide a rationale. A social bubble refers to a small, clearly defined group of people that agree to limit their social contacts to only those within the bubble which should be no larger than ten. Social bubbles would include roommates, sailing partners, training partners, and possibly coaches. Included in the social bubble, would be everyone living in the same dwelling, using the same bathroom and kitchen facilities. Creating new social bubbles during this event allowed competitors in the same boat, who are not in the same family, to have the requisite close contact when rooming together, and dining together, and while sailing together without face masks.
All coaches and athletes had to acknowledge that they were part of a bubble and agree to minimize close social contact with people outside of the bubble. People within the bubble were permitted to interact with one another without physical distancing or mask wearing although good hand hygiene was always encouraged. It is important to get agreement from everyone that they will join the social bubble and recognize the restrictions that are entailed in joining. That means they agree to join only one social bubble, and physically distance with anyone outside their social bubble.
Social bubbles also allowed for more rapid contact tracing in the event of a case of COVID-19 within a social bubble and would include anyone that had come into close contact with members of that social bubble.
Another component of physical distancing, which was initiated by the coaches and athletes, was to stagger the location of the boats within the boat park, rather than lined up like cars in a parking lot. This provided a three-meter distance between boats during rigging, derigging, and maintenance.
Hand Hygiene
Frequent hand washing is cited as the primary weapon in the fight against the transmission of COVID-19 (Howard et al., 2020; Seres et al., 2021; Steinbrook, 2020), however, we use “hand-hygiene” as an all-inclusive term also used in the literature (Chen et al., 2020; Cheng et al., 2020a) to include handwashing with soap and water, and/or the use of various chemical hand sanitizers or wipes. As a rule, hand hygiene takes place in the privacy of a washroom or using a pocket bottle of sanitizer. It was not reasonable to attempt to measure hand hygiene simply by the number of times someone accessed the public hand sanitizer. Instead, the use of reminder signage and accessible stations was the extent to which hand hygiene was included. Seres et al. (2021) also recommend proper coughing and sneezing etiquette which is also hard to assess due to its random occurrence.
Efficacy of Facemask Use
Face coverings such as masks have become a major source of prevention in the spread of COVID-19. (Cheng et al. 2020a; Clark et al. 2020) There has been considerable recent research addressing some of the issues on how COVID-19 is spread, whether it is airborne or droplet based, and what types of face coverings are most effective. (Fisher et al., 2020; Sickbert-Bennet et al., 2020). The general consensus at time of writing is that COVID-19 is spread primarily by droplet or micro-droplets which can travel multiple meters following an unobstructed cough or sneeze or even loud speaking or singing (Asadi et al. 2020a). There is also evidence that particles in the form of fomites, which can survive for extended periods of time on surfaces may subsequently be spread by touch. However, this is probably less common (Kanamori, 2020).
COVID-19 has energized a stream of research on the efficacy and compliance of facemask use to prevent the spread of the virus. Before mandating mask use, it was important to peruse the research literature to determine if there was adequate support for mandating that athletes make such a departure from their normal routine.
Airborne transmission of infectious respiratory diseases involves the emission of microorganism-containing aerosols and droplets during various expiratory activities (e.g., breathing, talking, coughing, and sneezing). Transmission of viruses in emitted droplets and aerosols to susceptible individuals may occur via physical contact after deposition on surfaces, reaerosolization after deposition, direct deposition of emitted droplets on mucosal surfaces (e.g., mouth, eyes), or direct inhalation of virus-laden aerosols (Asadi et al. 2020b, p. 1).
Liu & Zhang (2020) support the use of facemasks to reduce transmission of a virus when individuals must interact with one another and are not within the same social bubble.
The face mask that one person wears to reduce the potential release of droplets that contain virus complements the mask that another person wears to reduce the risk of inhaling these droplets. The consistent, correct, and universal wearing of face masks increases the benefit for individuals, and for all. This is neither rocket science nor a political statement. It is common sense and responsible behavior (Steinbrook, 2020 p. 470).
There had been concern voiced in the media, and by the public, that exercising while wearing a facemask could reduce available oxygen by trapping air thus preventing adequate carbon dioxide exchange. Hopkins et al. (2020) found mask wearing to “have small and often difficult-to-detect effects on [the work of breathing], blood gases and other physiological parameters during physical activity, even with heavy/maximal exercise” (p. 405). Although not required, if an athlete chose to wear a facemask, while on the water, during training and/or competition, there is no indication that it would impair performance.
The term facemask has come to represent a wide range of devices that could potentially be used to reduce aerosol transmission. There is also a wide range of commercially produced personal protective equipment (PPE) that could be used by athletes during training and competition, but due to the limited supply and higher demand it was difficult to specify specific PPE. Significant variability in the efficacy of face coverings has also been demonstrated in the literature (Fischer et al. 2020) which support either medical face masks or multiple ply (two layers or greater) close knit cloth masks.
Hopkins et al. (2020) noted that a variety of options were available from tight-fitting industrial and healthcare standard respirators, which would be inappropriate for sport use, to surgical masks, homemade or store-bought fabric masks, and loose-fitting bandanas or neck gaiters. Steinbrook (2020) concluded that a folded cotton bandana had approximately a 50% filtration efficiency and that improved fit between the mask and the wearer’s face increased filtration efficiency, such as through use of an aluminum nose bridge. The medical team deemed it prudent to investigate alternative options.
There is also debate about who the mask is protecting. Pre-COVD-19, in non-health related settings, such as industrial applications, the use of facemasks have focused on protecting the wearer from aerosol and particulate inhalation, so the emphasis was the protection of the wearer. “The most common application in modern medicine is to provide protection to the wearer (e.g., first responders), but surgical facemasks were originally introduced to protect surrounding persons from the wearer” (Fischer et al. 2020, p. 1).
The prevailing sentiment amongst the medical personnel on-site was that mask wearing was required to protect the athletes from one another and the coaching staff, any of whom may be carrying the virus yet be asymptomatic at the time. Cheng et al. (2020b) suggest that the emphasis needs to change to one of the wearers protecting others from respiratory droplets due to the potential for infection before symptoms are obvious or from asymptomatic carriers of the virus. They also note the opportunity to carry out research on compliance during a pandemic was not possible previously. Clapp et al. (2020) confirm that facemasks must completely cover the nose and mouth to be an effective intervention for preventing transmission of the virus. Appropriate fitting and usage of facemasks was a critical component of the assessment.
Assessing the level of compliance through observation was easiest for mask use compliance. A simple glance around the venue would quickly determine the number of noncompliant individuals.
Additional Benefits of Facemask Use
There has been concern voiced that compulsory facemask use emphasizes potentially counterproductive effects from incorrect use and a false sense of security. The improper use of masks can be mitigated with training. The argument that facemasks give individuals a false sense of security is dispelled by Betsch et al. (2020), Cheng et al. (2020b), Clapp et al. (2020), Howard et al. (2020) and Seres et al. (2021). Howard et al. (2020) confirm that handwashing combined with universal mask wearing reduces the spread of respiratory viruses but noted a significant secondary benefit being the visual reminder to others of the pandemic to increase compliance with unspoken social pressure. Seres et al. (2021) “show that individuals keep a significantly larger distance from someone wearing a face mask than from an unmasked person” (p. 139) which is aided by “a potential bias toward socially desirable behaviors” (p. 141).
Wearing a mask is a form of social contract which provides motivation to group members who would otherwise be noncompliant. Betsch et al. (2020) noted “compliant people perceive each other more positively, and noncompliance is socially punished” (p. 21852). Mask wearing by everyone involved was critical to the success of the event and high levels of compliance by all those involved in the training and competition would be of particular importance for the protection of coaches and administrators present (Cheng et al., 2020b; Clapp et al., 2020). Betsch et al. (2020) based their results on self-reported data whereas our results were grounded in real-life observations. Simply put, “masks help people keep their droplets to themselves” (Howard et al., 2020, p. 2).
Equipment Contamination Concerns
Concern was expressed regarding equipment contamination from an asymptomatic athlete or coach. Ratnesar-Shumate et al. (2020) determined that; “Ninety percent of infectious virus was inactivated every 6.8 minutes in simulated saliva and every 14.3 minutes in culture media when exposed to simulated sunlight representative of the summer solstice at 40°N latitude at sea level on a clear day” (p. 214). The medical team was satisfied that the likelihood of the virus surviving on equipment for any meaningful portion of time was minimal. Considering equipment is almost entirely synthetic material (fiberglass, stainless steel, anodized aluminum, various plastics, nylon, dacron, and mylar) and any wood components are coated in several layers of polyurethane, boats and equipment are unlikely to serve as significant fomites.
Coaching staff worked closely with the local Public Health Unit, municipality and, the sport’s COVID-19 Medical Task Force to ensure everything was done to make the event as safe and successful as possible during these challenging times. The literature review supported the COVID-19 restrictions and guided the event organizers’ implementation of the protocols.
The Event
The intent of the event was to create an elite level racing environment to focus on honing and maintaining racing skills for Olympic aspirants as a replacement for attending international competitions during a time when was it was not possible due to international travel restrictions. This case-study was to assess the efficacy of virus mitigation strategies to maintain training of elite athletes and avoid complete cessation of their programs. Coaches noted this was critical at the elite level both from a skill maintenance perspective and for mental health and stress reduction.
COVID-19 Constraints
Considering the research conducted, and to comply with local, regional, and provincial health authorities, the coaches, on-site at the event, developed several criteria that had to be met within the boat park and during the event, which included:
i) Masks to be worn at all times when on land by all participants, coaches, and staff.
ii) 2-meter social distancing to be maintained at all times by those, not in a specific “bubble” (i.e., a crew of 2 for a two-person boat).
iii) Daily attestation confirming no COVID-19 symptoms (see Appendix B).
iv) Daily temperature checks of all participants, coaches, and staff.
v) On-site washroom facilities.
vi) On-site hand sanitizing stations.
vii) A separation of 3 meters between boats when they were being rigged and de-rigged or during the launch/recovery process.
viii) No “visitors” in the boat park.
ix) An on-site source of drinking water.
x) Regatta staff stay on-site whenever training/racing was underway and during rigging and de-rigging.
xi) Controlled entry and egress to the boat park.
xii) No "rafting together" on the water (i.e., boats could not come alongside one another between races/exercises, which included coach boats).
xiii) Briefing and de-briefing was conducted via Zoom meetings as were protests.
xiv) Any individual or coach who became symptomatic during the event had to withdraw and not come to the site until cleared of COVID-19 as would any member of their social bubble.
xv) Any person with a positive COVID-19 test had to withdraw permanently as well as all members of their social bubble.
Despite these restrictions and precautions, there was considerable interest from a large number of athletes and coaches to participate in this event.
Athletes travelled from across Canada to attend this event although the majority were from central Canada. Few athletes travelled by aircraft, some chose to travel by automobile from afar to minimize the risk of contracting disease associated with travelling.
The Setting
The setting for the event was held at a venue built specifically for Olympic sailing events due to its water and wind characteristics, making it a favorable place to sail and compete. The site has a grassy area which was roped off to the public and housed 28 single handed sailboats and 16 double handed sailboats. The area reserved for the single-handed boats was 20 by 55 meters (1,100 square meters) and the area for the double-handed boats was 18 by 25 meters (450 square meters) which was ample space to store the boats overnight and then move them in the morning so that there was always a minimum of three meters between boats to ensure that the two-meter physical distancing between athletes and coaches could be maintained during the rigging process. The launch site was 60 meters from the controlled area. Volunteers, wearing protective gloves and masks, were on hand to assist with launching and the return to shore after each day of sailing to avoid athletes having to help each other launch and retrieve the boats.
In all, there was a maximum of 60 athletes on-site at any one time as well as up to 10 coaches and a further 10 – 15 staff/volunteers (officials, audit staff, support personnel, administrators, etc.) for a total of up to 85 people. Ages ranged from 15 to 65, with the majority being between ages 15 and 25.
The nine-day event schedule was set in such a way that the doublehanded athletes competed on days one through four and days six through nine. The female singlehanded athletes competed on days one through four, while the male singlehanded athletes competed on days six through nine. Day five was reserved as a recovery day for the doublehanded sailors and a transition day from female to male for the singlehanded sailors. This schedule ensured that there were never more than 46 competitors in the boat park area at any given time.
The female singlehanded athletes completed twelve races and male singlehanded athletes completed fifteen races over four days. Both male and female doublehanded athletes completed twenty-four races over eight days.
We found that a hands-on approach with on-site volunteers providing constructive reminders, equipped with spare masks and available to answer questions was both practical and impactful. Such considerations would be important in replicating these results.
The protocol and controlled environment were limited to the sailing venue. We did not control what the athletes were doing after sailing with respect to living arrangements, restaurants, or evening outings. Athletes were provided guidelines and the Kingston area regional Public Health Authority had been proactive in providing clear guidance to restaurant owners and hotels that would have been visited by the sailors. This is very much in accordance with the real-life scenarios of any amateur event.
Audit Measures
To monitor behavior, and ensure compliance, audits were performed daily on an audit form (see Appendix A) examining several metrics which included:
i) PPE and hand sanitizer supplies
ii) Attestation (Appendix B) and daily temperature checks (touchless thermometer)
iii) Daily attendance record to permit contact-tracing if required
iv) Bathroom facilities
v) Compliance with mask-wearing
vi) Compliance with physical distancing
vii) Compliance with boat distancing
Metrics v, vi and vii were collected whenever the athletes and coaches were onshore in the controlled area. The audit process was applied randomly to ensure ongoing compliance and ranged between 15 and 30-minute intervals. The process was modeled after the infection prevention and control processes used in most hospitals and other healthcare settings in Canada when auditing compliance of healthcare workers with PPE utilization (mask use and hand hygiene). Audits of physical resources such as bathroom facilities, hand sanitizing stations, potable water for the athletes, and security were done daily at the beginning of each day.
Data Collection
Auditors were on site daily and were not affiliated with the regatta management nor the administrative process. All auditors had to abide by the same COVID-19 screening protocols as the athletes, coaches, and regatta/training personnel. In all there were 2,567 separate observations that were documented using the audit tool to determine compliance over the entire nine days of the event (see Appendix A).
Athlete compliance was measured both within the boat park as well as during the transition stage from boat park to the launch ramp, when launching in the morning and the reverse in the evening during the return to shore. Compliance was also measured during the rigging of the boats when increased space (three meters) was required between boats to enable the athletes to safely walk around their boats without violating the two-meter rule with an athlete rigging an adjacent boat.
Outcomes
The two key performance metrics to ensure the safety of the athletes which were monitored were the wearing of masks and physical distancing.
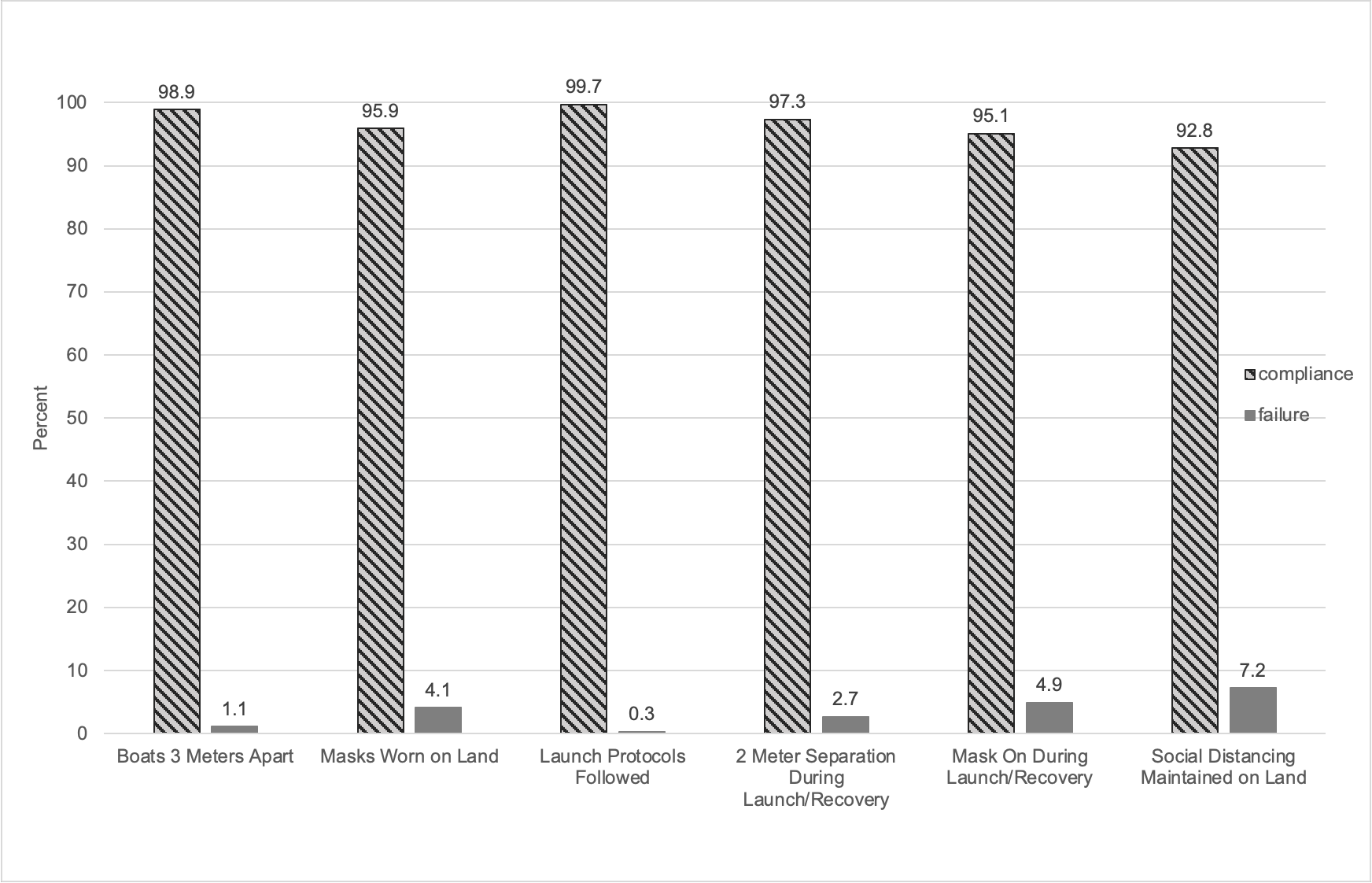
Mask Use
The supplied ASTM level 1 surgical masks were mandatory for all athletes, coaches, staff, and auditors when on land and specifically in the boat park. Wearing of masks on the water is not advisable. The wet environment reduces the efficacy of the mask and possibly creates a safety concern. Athletes need to transition out of wearing masks before entering the water and organizers provided reusable sealed plastic bags to athletes to help protect the mask properties during the sporting activity. These racing craft do not provide dry spaces, so the athletes had to retrieve their masks as they transitioned back to land at the end of the day’s competition while handling their boats on the ramp. A failure in mask use was documented when either a mask was not worn or worn improperly (i.e., the nose and/or mouth were exposed). Furthermore, on occasion when some athletes decided to supplant the provided surgical masks with other single layer face coverings (such as buffs or bandanas) was also deemed a failure as the efficacy of these in droplet control has been recently questioned by several researchers (Asadi et al. 2020b; Clapp et al. 2020; Fischer et al. 2020; Sickbert-Bennett et al. 2020). In each case of a failure being recorded the athlete was also provided corrective advice. Compliance for the wearing of a mask was found to be exceptionally high when in the boat park and only slightly lower during the transition phases to and from the launch area (see Figure 1).
Physical Distancing
Physical distancing was defined as being two meters away from the next closest person except when with someone from a person’s own “bubble”. Bubbles were usually either two athletes sailing in the same boat plus their coach or a single athlete in the case of a single person boat such as the Laser and that athlete’s coach. For the most part, physical distancing was maintained in the boat park during the rigging and de-rigging process and during launch and recovery (see Figure 1).
Figure 1
Compliance with COVID-19 Protocols Days 1–9.
Discussion
While mask wearing compliance within the public varies between a low of 40 percent and a high of 60 percent, we found the athletes to be highly motivated and demonstrated compliance rates of 95.9% on land and 95.1% during launch and recovery. It is not surprising that the compliance during launch and recovery was lower as it was not infrequent that a sailor would land and find that his or her mask was wet or damaged or forget to put it on immediately upon stepping ashore. This was ultimately partially resolved by having a volunteer at the water’s edge with a supply of masks to provide one to any athlete who landed without a mask, or with a damaged or soiled mask. Based on discussions with both athletes and coaches we attribute the high compliance with mask wearing, at a level that rivaled that seen in the health care settings, to the motivation of the athletes by their coaches as well as the presence of auditors on site. Success here could open the opportunities for future similar events.
Physical distancing was also maintained at a high level, again due in part to the presence of an audit team and vigilance on the part of the coaches. It is worth noting that the physical distancing during launch and recovery was superior to that in the boat park itself (97.3% versus 92.1%). It is postulated that this was a in part a function of the mechanics of launching of only one or two boats at a time with the space needed to physically launch a boat on the launch ramp as well as the absence of any “socializing” during this phase of the process. A secondary cause for a perceived lower compliance with social distancing in the boat park was the difficulty in accurately identifying “social bubbles” by the auditors since they were unfamiliar with the athletes, coaches, and teams from the same club. It was not infrequent that a violation was identified when in fact the third person may have been a coach or other team member from the same “bubble”. This could be alleviated in future by having all team members from a single bubble wear some article of clothing (i.e., a “bib”) of the same colour such that it would be easier to readily identify individual “bubbles” and violations from a distance. In this study, the number of violations of social distancing was likely over-stated when the athletes were in the boat park.
One and Two-week follow-up
Every athlete, and coach was contacted at the seven- and fourteen-day interval following the event to determine if there had been any need to test for COVID-19 based on symptoms. In all, 60 athletes and 10 coaches were contacted as well as the support staff who participated. At day seven, three individuals underwent COVID-19 testing of which one person was symptomatic and two were asymptomatic and tested for other reasons (employment, travel etc.). All three tested negative and a non-COVID-19 diagnosis was assigned to the one individual who had symptoms. By day 14, three more individuals had been tested. All were asymptomatic and all three also had negative COVID-19 swabs.
Conclusion
This experience demonstrated that it is possible and safe to operate training and a competitive regatta in the setting of COVID-19. We recommend that masks be worn at all times by all athletes, coaches, and support staff and that physical distancing of two meters is maintained. The use of “bubble identifiers” would aid greatly in monitoring physical distancing for the on-land component. We found excellent compliance the daily self-reporting and attestation form completion and with all virus mitigation measures including hand hygiene with this motivated group of high-performance athletes. It is our hope that this event may be used as a template to assist in running safe training and competitive events during the COVID-19 pandemic and beyond. Outdoor sports such as many winter alpine events (skiing and other sliding sports), cross-country skiing etc. and summer events like rowing, canoe/kayak, etc. could use this template to plan and execute training and competitions in a safe yet functional manner ensuring Olympic athletes maintain their training and competition readiness while simultaneously beginning the preparation and mentorship of the next generation of Olympic athletes. A thorough debrief of the event has been done with the organizing staff and the two medical officers who were on site. Any conclusion here should be made in consideration of the timing of this event, the prevalence of COVID-19 at the time of the event both locally in Kingston Ontario and in Canada during the month of August 2020.
Acknowledgements
We would like to thank Katie Sweeting, Mike Milner, and Don Adams of Sail Canada for their tremendous efforts in coordinating the event, the collection of data, and ensuring this regatta was safe for everyone involved.
References
Asadi, S., Bouvier, N. M., Wexler, A. S., & Ristenpart, W. D. (2020a). The coronavirus pandemic and aerosols: Does COVID-19 transmit via expiratory particles? Aerosol Science and Technology, 54(6), 635-638. https://doi.org/10.1080/02786826.2020.1749229
Asadi, S., Cappa, C. D., Barreda, S., Wexler, A. S., Bouvier, N. M., & Ristenpart, W. D. (2020b). Efficacy of masks and face coverings in controlling outward aerosol particle emission from expiratory activities. Nature Research Scientific Reports, 10(1), 1-13. https://www.nature.com/articles/s41598-020-72798-7
Betscha, C., Korn, L., Sprengholz, P., Felgendreff, L., Eitze, S., Schmid, P., & Böhm, R. (2020). Social and behavioral consequences of mask policies during the COVID-19 pandemic. Proceedings of the National Academy of Sciences of the United States of America, 117(36). 21851-21853. https://www.pnas.org/content/pnas/117/36/21851.full.pdf
Chen, X., Ran, L., Liu, Q., Hu, Q., Du, X., & Tan, X. (2020). Hand hygiene, mask-wearing behaviors and its associated factors during the COVID-19 epidemic: A cross-sectional study among primary school students in Wuhan, China. International Journal of Environmental Research and Public Health, 17(8), 2893. https://doi.org/10.3390/ijerph17082893
Cheng, K. K., Lam, T. H., & Chi Chiu Leung, C. C. (2020a). Wearing face masks in the community during the COVID-19 pandemic: Altruism and solidarity. The Lancet 399(10336), e39-e40. https://doi.org/10.1016/S0140-6736(20)30918-1
Cheng, V. C-C., Wong, S-C., Chuang, V. W-M., So, S. Y-C., Chen, J H-K., Sridhar, S., To, K. K-W., Chan, J. F-W, Hung, I. F-N., Ho, P-L., & Yuen, K-Y. (2020b). The role of community-wide wearing of face mask for control of coronavirus disease 2019 (COVID-19) epidemic due to SARS-CoV-2. Journal of Infection 81(1),107-114. https://doi.org/10.1016/j.jinf.2020.04.024
Clapp, P. W., Sickbert-Bennett, E. E., Samet, J. M., Berntsen, J., Zeman, K. L., Anderson, D. J., Weber, D. J., & Bennett, W. D. (2020). Evaluation of cloth masks and modified procedure masks as personal protective equipment for the public during the covid-19 pandemic. Journal of the American Medical Association: Internal Medicine 181(4), 463-469. doi:10.1001/jamainternmed.2020.8168
Clark, C., Davila, A., Regis, M., & Kraus, S. (2020). Predictors of COVID-19 voluntary compliance behaviors: An international investigation. Global Transitions 2, 76-82. https://doi.org/10.1016/j.glt.2020.06.003
Eikenberry, S. E., Mancuso, M., Iboi, E., Phan, T., Eikenberry, K., Kuang, Y., Kostelich, E., & Gumel, A. B. (2020). To mask or not to mask: Modeling the potential for face mask use by the general public to curtail the COVID-19 pandemic. Infectious Disease Modelling, 5, 293-308. https://doi.org/10.1016/j.idm.2020.04.001
Fischer, E. P., Fischer, M. C., Grass, D., Henrion, I., Warren, W. S., & Westman, E. (2020) Low-cost measurement of facemask efficacy for filtering expelled droplets during speech. Science Advances, 6(36), eabd3083. doi:10.1126/sciadv.abd3083
Hopkins, S. R., Dominelli, P. B., Davis, C. K., Guenette, J. A., Luks, A. M., Molgat-Seon, Y., Sá, R. A., Sheel, A. W., Swenson, E. R., & Stickland, M. K. (2020). Facemasks and the cardiorespiratory response to physical activity in health and disease. Annals of the American Thoracic Society, 18(3),399-407. https://doi.org/10.1513/AnnalsATS.202008-990CME
Howard, J., Huang, A., Li, Z., Tufekci, Z., Zdimal, V., van der Westhuizen, H-M., von Delft, A., Price, A., Fridmand, L., Lei-Han Tang, L-H., Tang, V., Watson, G. L., Bax, C. E., Shaikh, R., Questier, F., Hernandez, D., Larry F. Chu, L. F., Christina M. Ramirez, C. M., & Rimoin, A. W. (2020, April 12). Face masks against COVID-19: An evidence review. Proceedings of the National Academy of Sciences of the United States of America, 118(4), e2014564118. https://doi.org/10.1073/pnas.2014564118
Kanamori, H. (2020). Rethinking environmental contamination and fomite. transmission of SARS-CoV-2 in the healthcare. Journal of Infection, 82(1), E17-E18. https://doi.org/10.1016/j.jinf.2020.08.041
Liu, X. & Zhang, S. (2020) COVID-19: Face masks and human-to-human transmission. Influenza and Other Respiratory Viruses, 14(4), 472–473. doi:10.1111/irv.12740
Ratnesar-Shumate, S., Williams, G., Green, B., Krause, M., Holland, B., Wood, S., Bohannon, J., Boydston, J., Freeburger, D., Hooper, I., Beck, K., Yeager, J., Altamura, L. A., Biryukov, J., Yolitz, J., Schuit, M., Wahl, V., Hevey, M., & Dabisch, P. (2020). Simulated sunlight rapidly inactivates SARS-CoV-2 on surfaces. The Journal of Infectious Diseases, 222(2), 214-222. https://doi.org/10.1093/infdis/jiaa274
Seres, G., Balleyer, A., Cerutti, N. Danilov, A., Friedrichsen, J., Liu, Y., & Süer, M. (2021) Face masks increase compliance with physical distancing recommendations during the COVID-19 pandemic. Journal of the Economic Science Association, 7, 139–158. https://doi.org/10.1007/s40881-021-00108-6
Sickbert-Bennett, E.E., Samet, J. M., Clapp, P. W., Chen, H., Berntsen, J., Zeman, K. L., Tong, H., Weber, D. J., & Bennett, W.D. (2020). Filtration efficiency of hospital face mask alternatives available for use during the COVID-19 pandemic. Journal of the American Medical Association: Internal Medicine,180(12), 1607-1612. doi:10.1001/jamainternmed.2020.4221
Steinbrook, R. (2020) Filtration efficiency of face masks used by the public during the COVID-19 pandemic. Journal of the American Medical Association: Internal Medicine, 181(4), 470. doi:10.1001/jamainternmed.2020.8234
*Address correspondence to:
David Telles-Langdon, Ph.D.
Kinesiology and Applied Health
University of Winnipeg
Manitoba, Canada
Email: d.telles-langdon@uwinnipeg.ca
![]()
Journal of Kinesiology and Wellness © 2022 by Western Society for Kinesiology and Wellness is licensed under CC BY-NC-ND 4.0.