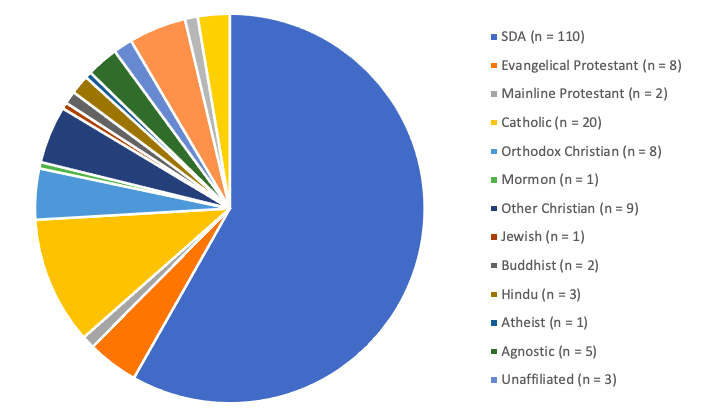
Figure 1
Religious Affiliation
A Comparison of Health Locus of Control and Physical Activity among Seventh-day Adventists and non-Seventh-day Adventists
Kimberly E. Feiler & Han Gia Ngo
Health and Exercise Science Department, La Sierra University
Submitted May 2022 | Accepted in final form July 2022
Feiler & Ngo. This study aimed to assess the correlation between physical activity (PA) levels and health locus of control (HLOC: internal, external-chance, external-powerful others, God/God locus of health control) among Seventh-day Adventists (SDA) and non-SDAs. The sample of this study included 185 individuals aged 22 to 81 who were employed by or attending an SDA affiliated higher education institution during the 2020-2021 academic school year. By completing the survey voluntarily, the participants provided their PA level and information regarding their HLOC. To analyze the impact of HLOC on PA, a multiple regression analysis was conducted. While overall results for a majority of respondents showed high levels of PA, SDAs reported statistically significant lower PA than did non-SDAs. HLOC (internal, external-chance, external-powerful others, God/God locus of health control) was not a significant predictor for PA.
Key Words: Seventh-day Adventist, physical activity, health locus of control, God locus of health control.
Introduction
Physical inactivity has become the world’s fourth leading cause of death (World Health Organization [WHO], 2019). This lack of physical activity (PA) contributes to multiple chronic health problems, such as high blood pressure, heart disease, diabetes, weak bones and muscles, poor weight management, and even some cancers (WHO, 2019). Within the United States, almost 80% of adults do not achieve enough PA (Centers for Disease Control and Prevention [CDC], 2017), which has resulted in annual healthcare costs of about $90 billion (Carlson et al., 2015). Even though the CDC (2017) recommends adults obtain 150 minutes per week of aerobic exercise and 2 days per week of muscular strengthening exercise, the average American adult has a difficult time following such recommendations.
Much research has been done on PA within selected groups of individuals, including those who are part of religious groups. With more than 92% of Americans identifying with a religion, it is important to question if there is something there that contributes to PA engagement, or lack thereof (Pew Research Center, 2020). Unfortunately, religiously-connected people tend to get significantly less PA than the recommendations (Ahrenfeldt et al., 2018; Aljayyousi et al., 2019; Banerjee et al., 2017; Geller et al., 2019; Joseph et al., 2017; Lycett, 2015; Nathenson & Wen, 2013; Park et al., 2018; Pullins et al., 2018; Rabiepoor et al., 2019; Thomson et al., 2015; Tristão Parra et al., 2018; Waters et al., 2018; Williams et al., 2016). However, there is one group that appears to contradict these findings: Seventh-day Adventists (SDAs).
SDAs are Protestant Christians who are distinguished by the belief in the second coming of Jesus Christ and the observance of the Sabbath – the seventh day of the week in the Hebrew calendar (General Conference of SDAs (Seventh-day Adventists) [GC], 2019). The SDA belief system encourages the practice of healthy lifestyles, including a diet that is mainly plant-based and avoids animal products that are deemed to be “unclean” according to the Bible, regular PA, resting on Sabbath (Saturdays), worshiping, and engaging in social fellowship (GC, n.d.). One SDA hub is Loma Linda, CA, and has been labeled a “Blue Zone,” which is one of the areas around the world where people live the longest and healthiest lives (Buettner, 2010). Loma Linda is home to a flagship SDA medical school and hospital; the Loma Linda residents’ secrets for longevity were daily engagement in regular PA and belonging to a faith-based community where there is support for practicing the lifestyle recommendations of the SDA church (Buettner, 2010). Hence, there is a known correlation between PA and the health beliefs of those within the SDA faith. In Lindsted et al.’s (1991) longitudinal study of SDA men, they found that moderate levels of PA protected them from all causes of death, thereby delaying death to 95.6 years, as compared to the national average of 78.8 years (CDC, 2018). Acosta Enríquez et al. (2019) examined lifestyle behaviors of SDA and non-SDA adolescents and found no differences in PA levels, although those who participated in a sport had low body mass index levels. Koenig’s (2012) systematic review found that religiously-involved people exhibited a mostly positive relationship to obtaining adequate PA. There are many factors that influence PA and health beliefs; one such factor is health locus of control (HLOC).
HLOC refers to the position one takes in controlling one’s decisions for their own health. According to Wallston (Wallston et al., 1978; n.d., 1993, 2005), the three subcategories for HLOC are internal, external-chance, and external-powerful others. Internal HLOC indicates that health is in one’s own control. External-chance HLOC indicates that one believes their health is controlled by fate or luck. External-powerful others HLOC indicates that one believes their health is controlled by significant others, such as doctors, and/or God or individuals with a higher power. Wallston et al. (1999) expanded the HLOC category of external-powerful others and developed the God locus of health control (GLHC). This aimed to better understand how belief in God played a role in health control – how much does a person believe that God controls their health?
How HLOC shapes preventive health behavior, such as PA, has previously been studied in multiple population groups. Sak et al.’s (2013) study of college students’ health behaviors showed primarily internal HLOC with additional significant influence from external-powerful others. Similarly, Bennett et al. (2017) found that college students who used online and/or application health trackers were likely to have high HLOC scores for both internal and external-powerful others. Helmer et al. (2012) and Carlson and Petti (1989) all found young adult students with high internal HLOC had high PA, whereas those with high external-chance HLOC had low PA. Rongen et al. (2014) discovered that employees with high internal HLOC were likely to have high self-rated health yet low engagement in employee wellness programs. Anastasiou et al. (2015) found that adults with high internal HLOC were more likely than those with high external HLOCs to engage in adequate PA. Webb et al.’s (2012) study found that pregnant women were less likely to participate in PA if they had high external-chance HLOC scores. Moshki et al. (2014) found postpartum depressive women showed decreased external and increased internal HLOCs after four months of depression intervention. Thomas et al. (2016) determined that African American women had higher internal HLOC and increased PA at a 6-month follow-up of an intervention to improve lifestyle choices. Pudrovska’s (2015) longitudinal study found that as compared to men, women had more PA limitations and lower self-rated health, yet higher religiosity – which was associated with high internal HLOC.
Regarding GLHC and PA, Robinson and Wicks (2012) found African American women showed high GLHC and low levels of PA. Karvinen and Carr (2013) determined that GLHC scores were negatively associated with PA and internal HLOC, yet positively associated with both external HLOCs. Boyd and Wilcox (2020) discovered that college students who frequently attended religious services were likely to have high GLHC and external HLOC scores, and low internal HLOC scores.
It is important to note that no publications to date have addressed the combination of HLOC (internal, external-chance, external-powerful others, GLHC) and PA in a religiously-affiliated population. This study investigated the relationships between the independent variables (IV) of HLOC’s internal, external-chance, external-powerful others, and GLHC categories, and the dependent variable (DV) of PA. The null hypothesis stated that HLOC subscales would not significantly predict PA.
Methods
For this study, four pre-existing questionnaires were combined into one survey that was administered via email using PsychData: (1) International Physical activity (PA) Questionnaire (2002), which measures PA during leisure time, at work, and for transport within the last week, and has been reliably and validly correlated with accelerometer data (Kim et al., 2013; Macfarlane et al., 2011; Papathanasiou et al., 2009); based on Cohen’s guidelines a medium effect size (0.39) was found for total PA (Kim et al., 2013), good test-retest reliability and Spearman’s correlation for total PA (r = 0.35; Macfarlane et al., 2011), and intra-class correlation coefficients were high for total PA (0.84; Papathanasiou et al., 2009). Next, (2) the Multidimensional Health Locus of Control (Wallston et al., 1976) measures an individual’s level of belief regarding control factors over their health as internal, external-chance, and external-powerful others, and has shown to have moderate reliability with Cronbach alphas ranging from .60 - .75, and test-retest stability coefficients from .60 - .70 (Otto et al., 2011; Wallston, 1993). Then, (3) the God Locus of Health Control (GLHC; Wallston et al., 1999), which measures an individual’s level of belief that God is in control of their health, has shown strong alpha reliability at about .90 and has validly measured religious beliefs about health (r = .29 and .32, between GLHC scores and religious importance ratings, and r = .42 and .47, between GLHC and using religion to cope with pain; Mills et al., 2018; Murray et al., 2006; Robinson & Wicks, 2012; Wallston, 2005; Wallston et al., 1999). Last, (4) Short Form 36, which measures self-reported health-related quality of life (RAND Corporation, 2019), has shown to have established validity and reliability above 0.80 (Ware et al., 1993), and median relative precision at 0.93 (McHorney et al., 1992, 1994). None of the pre-existing questionnaires included demographic questions; such questions were added in and included age, gender, ethnicity, education level, marital status, household number, and religious affiliation. This article will focus on results from the first three questionnaires and the demographic element of religious affiliation.
From February through April 2021, the survey link was sent once to all individuals with active institutional email addresses at three SDA-affiliated higher education institutions, as the minimum number of respondents was met with a single email at each institution. These individuals were employed by or attending an SDA-affiliated higher education institution during the 2020-2021 academic school year. The respondents were informed about their voluntary participation and their right to withdraw from the study at any time. SPSS version 27 was used to analyze the data.
Results
A total of 313 initiated the survey but only 185 students, faculty, and staff from three SDA-affiliated institutions completed the self-response survey. Age of participants ranged from 22 to 81 years of age, 68% identified as female, and 59.5%% identified as SDA (see Figure 1). After collection, the data was analyzed using descriptive and inferential statistics. Multiple regression was conducted to examine the relationship between HLOC (internal, external-chance, external-powerful others, God/GLHC) and the self-reported PA levels among participants. The novel coronavirus SARS-CoV-2, which causes the COVID-19 infection, has had a profound effect on all aspects of society worldwide, including sporting events and training.
Figure 1
Religious Affiliation
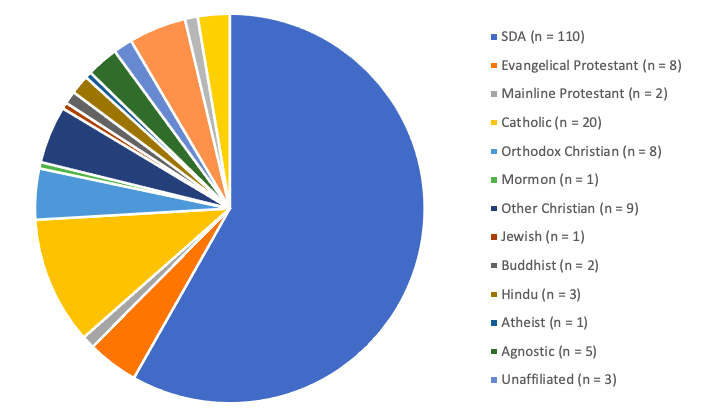
The regression showed that the model was not statistically significant (F(4, 165) = .329, p = .858, R2 = .008) and the null hypothesis was not rejected. The independent variables included in the model were not significant predictors of PA, meaning that no HLOC category had a significant impact on PA levels (see Table 1). However, the results showed that 66% of the participants reported high levels of PA (achieving at least 3,000 METS per week), 28% reported moderate levels of PA (at least 600 METS per week), and 5% reported low amounts of PA (less than 600 METS per week; see Table 2).
Table 1
Regression Analysis Results
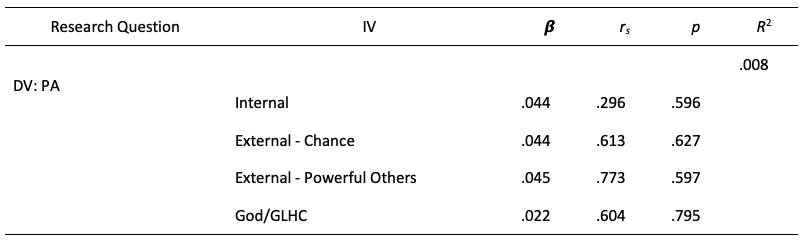
Table 2
PA Categories for Different Age Groups (Percentages Shown for Total of All Respondents)
Note. Table total percentage = 100%.
In comparing SDAs and non-SDAs, the results showed some differences. When compared to non-SDAs, SDA’s had significantly higher internal HLOC scores (t(182) = 2.251, p = 0.026, d = .338), which was a small effect. There were no significant differences between SDAs and non-SDAs for any other HLOC category (external-chance: (t(183) = -1.865, p = .064, d = -.279; external-powerful others: (t(183) = -2.274, p = .024, d = -.341; GLHC: (t(183) = -0.70, p = .944, d = -.010).
More than 60% of SDAs achieved a high amount of PA, while 75% of non-SDAs had a high amount (see Table 3). For moderate amounts of PA, 33% of SDAs whereas 22% of non-SDAs obtained moderate amounts. Almost 7% of SDAs and just under 3% of non-SDAs had a low amount of PA. SDAs had statistically significantly lower PA levels than did non-SDAs (t(169) = -2.883, p = 0.005, d = -.479), which was a moderate effect.
Table 3
PA for SDAs and Non-SDAs
![]()
Discussion
The results from this study showed that none of the HLOC subscales was a statistically significant predictor of PA, therefore we failed to reject the null. This finding is not consistent with previous studies which found a positive relationship between high internal HLOC and high PA levels, and a negative relationship between external-chance and/or external-powerful others and PA (Anastasiou et al., 2015; Carlson & Petti, 1989; Helmer et al., 2012; Karvinen & Carr, 2013; Rongen et al., 2014). In addition, the present study’s findings do not align with research that has shown those with high GLHC scores were less likely to engage in PA in any amount (Karvinen & Carr, 2013; Robinson & Wicks, 2012). These differences comparing past studies with the present study are addressed below.
In comparing HLOC of SDAs and non-SDAs, SDAs had higher internal scores, which indicates that they believe they have greatest control over their own health and health outcomes. This is not to say non-SDAs do not have high internal HLOC scores, simply that SDAs scored even higher. The high internal HLOC score for SDAs could be associated with the SDA belief that God empowers individuals to be in control of their lives, rather than leave things to chance, fate, or other influences. There were no other differences between SDAs and non-SDAs in the other categories for HLOC (external-chance, external-powerful others, God/GLHC). Although not part of this study, attendance at religious services has shown to be positively correlated to high GLHC scores (Boyd & Wilcox, 2020). This is an element that could be addressed in future studies.
The finding that more than half of participants engaged in moderate or high levels of PA was surprising yet consistent with Lindsted et al.’s (1991) study on SDAs. Koenig (2012) and Park et al. (2018) had each previously found that religious involvement and PA were positively correlated, although Acosta Enriquez et al. (2019) found no differences in PA levels when comparing religious and non-religious individuals. This study’s findings are a stark contrast to CDC (2017) reports that have indicated about 80% do not get enough PA. In addition, many other studies have shown that religiously-affiliated individuals do not obtain adequate PA (Aljayyousi et al., 2019; Banerjee et al., 2017; Geller et al., 2019; Joseph et al., 2017; McKenzie et al., 2015; Nathenson & Wen, 2013; Rabiepoor et al., 2019; Thomson et al., 2015; Tristão Parra et al., 2018; Waters et al., 2018; Williams et al., 2016). It is likely that the PA of this study’s sample is more greatly influenced by other, non-HLOC factors that were not part of this study, such as access to PA locations (indoor, outdoor), familial support, and previous positive PA experience, among other potential factors. One possible explanation might be related to the COVID-19 pandemic – Cheval et al. (2021) found that many individuals increased their leisure-time PA during shutdown, as compared to pre-pandemic levels, which showed to help reduce the negative impact of the stressful time on mental health.
It should be noted that while all respondents worked at or attended an SDA institution, most respondents (59.5%) identified as SDA and most of the remaining respondents identified with a different religion. Only 10.8% combined identified as either agnostic, atheist, unaffiliated, nothing in particular, or did not wish to respond – which could mean many things. With about 90% identifying with a religion, this is similar to the Pew Research Center’s (2020) previous finding that 92% of Americans identify as religiously-affiliated.
This study had a few limitations, including the failure to draw causal relationships between the investigated variables and the use of a self-report PA measurement tool, which is less accurate than accelerometers and can allow respondents to overestimate their actual PA (Downs et al., 2014; LeBlanc & Janssen, 2010; Troiano et al., 2007). With this in mind, PA levels in this study may have been lower than reported. In addition, there may have been other, non-HLOC, factors that influenced PA participation for this study’s participants, including time spent caring for family members or at work; physical limitations or illnesses; both religious and PA attitudes, beliefs, behaviors, and/or practices that were not investigated within this study; and the COVID-19 pandemic, which impacted health and the workplace, which required many people to work from home, and thereby changed the work-home dynamic and related physical and mental health. Specific religious factors for future studies could include religious service attendance, prayer, and views on the role of God/a higher power and sanctity of the human body.
Nevertheless, most of the participants in this study reportedly achieved high levels of PA and only 5% of the participants obtained insufficient PA. These findings contradicted previous studies which showed that many people of a religiously-affiliated group, such as SDAs, tend to not engage in adequate PA (Aljayyousi et al., 2019; Banerjee et al., 2017; Geller et al., 2019; Joseph et al., 2017; McKenzie et al., 2015; Nathenson & Wen, 2013; Rabiepoor et al., 2019; Thomson et al., 2015; Tristão Parra et al., 2018; Waters et al., 2018; Williams et al., 2016).
Conclusions
This study was conducted to examine the impact that HLOC (internal, external-chance, external-powerful others, God/GLHC) has on PA among those working at or attending SDA institutions of higher education. Although previous research found a positive correlation between HLOC and PA, the results from this study indicated that none of the HLOC subcategories is a significant indicator of PA. This suggests that other factors play a stronger role in influencing the high PA levels of the sample in this study, such as time spent caring for others, illness, religious beliefs, and PA beliefs, among others. Further research should be conducted to assess the relationship between HLOC and PA among SDAs when the settings of the study are not influenced by COVID-19, as well as using a non-subjective PA measurement tool, such as accelerometers.
References
Acosta Enríquez, M. E., Uribe Salas, F. J., Baek, J., Archbold, J. P. S., & Carrillo, G. (2019). Association between life-style behaviors and health outcomes in Adventist and non-Adventist adolescents in Mexico: A pilot study. BMC Public Health, 19, 1705. https://doi.org/10.1186/s12889-019-8042-0
Ahrenfeldt, L. J., Möller, S., Hvidt, N. C., & Lindahl-Jacobsen, R. (2018). Religiousness and lifestyle among Europeans in SHARE. Public Health (Elsevier), 165, 74–81. https://doi.org/10.1016/j.puhe.2018.09.009
Aljayyousi, G. F., Munshar, M. A., Al-Salim, F., Osman, E. R., & Abu Munshar, M. (2019). Addressing context to understand physical activity among Muslim university students: The role of gender, family, and culture. BMC Public Health, 19(1), 1–12. https://doi.org/10.1186/s12889-019-7670-8
Anastasiou, C. A., Fappa, E., Karfopoulou, E., Gkza, A., & Yannakoulia, M. (2015). Weight loss maintenance in relation to locus of control: The MedWeight study. Behavior Research and Therapy, 71, 40–44. https://doi.org/10.1016/j.brat.2015.05.010
Banerjee, A., Landry, M., Zawi, M., Childerhose, D., Price, J., Stephens, N., & Shafique, A. (2017). A pilot examination of a mosque-based physical activity intervention for south Asian Muslim women in Ontario, Canada. Journal of Immigrant & Minority Health, 19(2), 349–357. https://doi.org/10.1007/s10903-016-0393-3
Bennett, B. L., Goldstein, C. M., Gathright, E. C., Hughes, J. W., & Latner, J. D. (2017). Internal health locus of control predicts willingness to track health behaviors online and with smartphone applications. Psychology, Health, & Medicine, 22(10), 1224-1229. https://doi.org/10.1080/13548506.2017.1317354
Boyd, J. M., & Wilcox, S. (2020). Examining the relationship between health locus of control and God locus of health control: Is God an internal or external source? Journal of Health Psychology, 25(7), 931-940. https://doi.org/10.1177/1359105317739099
Buettner, D. (2010). The blue zones: Lessons for living longer from the people who’ve lived the longest. National Geographic Society.
Carlson, B. R., & Petti, K. (1989). Health locus of control and participation in physical activity. American Journal of Health Promotion, 3(3), 32–37. https://doi.org/10.4278/0890-1171-3.3.32
Carlson, S. A., Fulton, J. E., Pratt, M., Yang, Z., & Adams, E. K. (2015). Inadequate physical activity and health care expenditures in the United States. Progress in Cardiovascular Diseases, 57(4), 315–323. https://www.cdc.gov/nccdphp/dnpao/docs/carlson-physical-activity-and-healthcare-expenditures-final-508tagged.pdf
Centers for Disease Control and Prevention. (2017). Explore by location: California. Nutrition, physical activity, and obesity: Data, trends and maps. https://nccd.cdc.gov/dnpao_dtm/rdPage.aspx?rdReport=DNPAO_DTM.ExploreByLocation&rdRequestForwarding=Form
Centers for Disease Control and Prevention. (2018). Mortality data. National Center for Health Statistics - National Vital Statistics System. https://www.cdc.gov/nchs/nvss/deaths.htm
Cheval, B., Sivaramakrishnan, H., Maltagliati, S., Fessler, L., Forestier, C., Sarrazin, P., Orsholits, D., Chalabaev, A., Sander, D., Ntoumanis, N., & Boisgontier, M. P. (2021). Relationships between changes in self-reported physical activity, sedentary behaviour and health during the coronavirus (COVID-19) pandemic in France and Switzerland. Journal of Sports Sciences, 39(6), 699-704. https://doi.org/10.1080/02640414.2020.1841396
Downs, A., Van Hoomissen, J., Lafrenz, A., & Julka, D. L. (2014). Accelerometer-measured versus self-reported physical activity in college students: Implications for research and practice. Journal of American College Health, 62(3), 204–212. https://doi.org/10.1080/07448481.2013.877018
Geller, K., Harmon, B., Burse, N., & Strayhorn, S. (2019). Church-based social support’s impact on African-Americans’ physical activity and diet varies by support type and source. Journal of Religion & Health, 58(3), 977–991. https://doi.org/10.1007/s10943-018-0576-4
General Conference of Seventh-day Adventists. (n.d.). Vitality – Health. https://www.adventist.org/en/vitality/health/
General Conference of Seventh-day Adventists. (2019). Beliefs. https://www.adventist.org/en/beliefs/
Helmer, S. M., Krämer, A., & Mikolajczyk, R. T. (2012). Health-related locus of control and health behaviour among university students in North Rhine Westphalia, Germany. BMC Research Notes, 5, 703. https://doi.org/10.1186/1756-0500-5-703
International Physical Activity Questionnaire. (2002). IPAQ_English_self-admin_long.pdf. https://sites.google.com/site/theipaq/questionnaire_links
Joseph, R. P., Ainsworth, B. E., Mathis, L., Hooker, S. P., & Keller, C. (2017). Incorporating religion and spirituality into the design of community-based physical activity programs for African American women: A qualitative inquiry. BMC Research Notes, 10(1), 506. https://doi.org/10.1186/s13104-017-2830-3
Karvinen, K. H., & Carr, L. J. (2013). Does the perception that God controls health outcomes matter for health behaviors? Journal of Health Psychology, 19(4), 521–530. https://doi.org/10.1177/1359105312474914
Kim, Y., Park, I., & Kang, M. (2013). Convergent validity of the international physical activity questionnaire (IPAQ): Meta-analysis. Public Health Nutrition, 16(3), 440–452. https://doi.org/10.1017/S1368980012002996
Koenig, H. G. (2012). Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry. https://doi.org/10.5402/2012/278730
LeBlanc, A. G. & Janssen, I. (2010). Difference between self-reported and accelerometer measured moderate-to-vigorous physical activity in youth. Pediatric Exercise Science, 22(4), 523–534.
Lindsted, K. D., Tonstad, S., & Kuzma, J. W. (1991). Self-report of physical activity and patterns of mortality in Seventh-day Adventist men. Journal of Clinical Epidemiology, 44(4–5), 355–364. https://doi.org/10.1016/0895-4356(91)90074-j
Lycett, D. (2015). The association of religious affiliation and body mass index (BMI): An analysis from the health survey of England. Journal of Religion & Health, 54(6), 2249–2267. https://doi.org/10.1007/s10943-014-9975-3
Macfarlane, D., Chan, A., & Cerin, E. (2011). Examining the validity and reliability of the Chinese version of the international physical activity questionnaire, long form (IPAQ-LC). Public Health Nutrition, 14(3), 443–450. https://doi.org/10.1017/S1368980010002806
McHorney, C. A., Ware, J. E., Rogers, W., Raczek, A. E., & Lu, J. F. R. (1992). The validity and relative precision of MOS short- and long-form health status scales and Dartmouth COOP charts: Results from the medical outcomes study. Medical Care, 30(5), MS253–MS265. https://www.doi.org/10.1097/00005650-199205001-00025
McHorney, C. A., Ware, J. E., Lu, J. F. R., & Sherbourne, C. D. (1994). The MOS 36-item short-form health survey (SF-36®): III, tests of data quality, scaling assumptions and reliability across diverse patient groups. Medical Care, 32(4), 40-66.
McHorney, C. A., Ware, J. E., Rogers, W., Raczek, A. E., & Lu, J. F. R. (1992). The validity and relative precision of MOS short- and long-form health status scales and Dartmouth COOP charts: Results from the medical outcomes study. Medical Care, 30(5), MS253-MS265.
McKenzie, M. M., Modeste, N. N., Marshak, H. H., & Wilson, C. (2015). Religious involvement and health-related behaviors among black Seventh-day Adventists in Canada. Health Promotion Practice, 16(2), 264–270. https://doi.org/10.1177/1524839914532812
Mills, S. D., Arredondo, E. M., Perez, L. G., Haughton, J., Roesch, S. C., & Malcarne, V. L. (2018). Psychometric properties of the God locus of health control scale in churchgoing Latinas. Hispanic Journal of Behavioral Sciences, 40(2), 227–239. https://doi.org/10.1177/0739986318762464
Moshki, M., Beydokhti, T. B., & Cheravi, K. (2014). The effect of educational intervention on prevention of postpartum depression: An application of health locus of control. Journal of Clinical Nursing, 23, 2256-2263. https://doi.org/10.1111/jocn.12505
Murray, T. S., Goggin, K., & Malcarne, V. L. (2006). Development and validation of the alcohol-related God locus of control scale. Addictive Behaviors, 31(3), 553-558.
Nathenson, S. L., & Wen, M. (2013). Religiousness, physical activity and obesity among older cancer survivors: Results from the health and retirement study 2000-2010. Journal of Religion & Spirituality in Society, 2(3), 129–144.
Otto, C., Bischof, G., Rumpf, H. J., Meyer, C., Hapke, U., & John, U. (2011). Multiple dimensions of health locus of control in a representative sample: Ordinal factor analysis and cross-validation of an existing three and a new four factor model. BMC Medical Research Methodology, 11, 114. https://doi.org/10.1186/1471-2288-11-114
Papathanasiou, G., Georgoudis, G., Papandreou, M., Spyropoulos, P., Georgakopoulos, D., Kalfakakou, V., & Evangelou, A. (2009). Reliability measures of the short international physical activity questionnaire (ipaq) in Greek young adults. Hellenic Journal of Cardiology, 50(4), 283–294.
Park, C. L., Waddington, E., & Abraham, R. (2018). Different dimensions of religiousness/spirituality are associated with health behaviors in breast cancer survivors. Psycho-Oncology, 27(10), 2466-2472. https://doi.org/10.1002/pon.4852
Pew Research Center. (2020). Religious landscape study. Religion and Public Life. https://www.pewforum.org/religious-landscape-study/
Pudrovska, T. (2015). Gender and health control beliefs among middle-aged and older adults. Journal of Aging and Health, 27(2), 284-303. https://doi.org/10.1177/0898264314549659
Pullins, C. T., Penheiter, S., Buras, M. R., Brewer, L. C., Seele, P. C., White, R. O., Willis, F. B., Poole, K., Albertie, M. L., Chamie, C., Allen, A. M., & Kelly, M. (2018). Health behaviors and preventive healthcare utilization among African-American attendees at a faith-based public health conference: Healthy churches 2020. Journal of Religion & Health, 57(6), 2538–2551. https://doi.org/10.1007/s10943-018-0667-2
Rabiepoor, S. Sadeghi, E., & Sayyadi, H. (2019). Spiritual health and physical activity among Iranian pregnant women. Journal of Religion & Health, 58(2), 506–515. https://doi.org/10.1007/s10943-017-0487-9
RAND Corporation. (2019). 36-item short form survey (SF-36). RAND Health Care. https://www.rand.org/health-care/surveys_tools/mos/36-item-short-form.html
Robinson, B. K., & Wicks, M. N. (2012). Religiosity, self-efficacy for exercise, and African American women. Journal of Religion and Health, 51(30), 854–864. https://doi.org/10.1007/s10943-010-9397-9
Rongen, A., Robroek, S. J., & Burdorf, A. (2014). The importance of internal health beliefs for employees’ participation in health promotion programs. Preventive Medicine, 67, 330–334. https://doi.org/10.1016/j.ypmed.2014.07.037
Sak, J., Wiechetek, M., Jarosz, M., Pawlikowski, J., Kapusta, A., Rejdak, L., & Ksiazek, P. (2013). Health behaviors and psychological health control types among university students. Polish Journal of Public Health, 123(3), 236-240. https://doi.org/10.12923/j.0044-2011/123-3/a.06
Thomas, V. G., Gaston, M. H., Porter, G. K., & Anderson, A. (2016). Prime time sister circles ® II: Evaluating a culturally relevant intervention to decrease psychological and physical risk factors for chronic disease in mid-life African American women. Journal of the National Medical Association, 108(1): 6-18. https://doi.org/10.1016/j.jnma.2015.12.001
Thomson, J. L., Goodman, M. H., & Tussing-Humphreys, L. (2015). Diet quality and physical activity outcome improvements resulting from a church-based diet and supervised physical activity intervention for rural, southern, African American adults. Health Promotion Practice, 16(5), 677–688. https://doi.org/10.1177/1524839914566851
Tristão Parra, M., Porfirio, G. J. M., Arredondo, E. M., & Atallah, A. N. (2018). Physical activity interventions in faith-based organizations: A systematic review. American Journal of Health Promotion, 32(3), 677–690. https://doi.org/10.1177/0890117116688107
Troiano, R. P., Berrigan, D., Dodd, K. W., Masse, L. C., Tilert, T., & McDowell, M. (2007). Physical activity in the United States measured by accelerometer. Medicine and Science in Sports and Exercise, 40, 181–188.
Wallston, K. A. (n.d.). Multidimensional health locus of control scale. https://nursing.vanderbilt.edu/projects/wallstonk/pdf/C19.pdf
Wallston, K. A. (1993). Multidimensional health locus of control (MHLC) scales. Vanderbilt University School of Nursing. https://nursing.vanderbilt.edu/projects/wallstonk/index.php
Wallston, K. A. (2005). Overview of the special issue on research with the multidimensional health locus of control (HLOC) scales. Journal of Health Psychology, 10(5), 619–621. https://doi.org/10.1177/1359105305055301
Wallston, B. S., Wallston, K. A., Kaplan, G. D., & Maides, S. A. (1976). Development and validation of the health locus of control (HLC) scale. Journal of Consulting and Clinical Psychology, 44(4), 580–585. https://doi.org/10.1037/0022-006X.44.4.580
Wallston, K. A., Wallston, B. S., & DeVellis, R. (1978). Development of multidimensional health locus of control (MHLC) scale. Health Education Monographs, 6, 160–170. https://doi.org/10.1177/109019817800600107
Wallston, K. A., Malcarne, V. L., Flores, L., Hansdottir, I., Smith, C. A., Stein, M. J., Weisman, M. H., & Clements, P. J. (1999). Does God determine your health? The God locus of health control scale. Cognitive Therapy and Research, 23(2), 131–142. https://nursing.vanderbilt.edu/projects/wallstonk/pdf/A71.pdf
Ware, J. E., Snow, K. K., Kosinksi, M., & Gandek, B. (1993). SF-36® health survey manual and interpretation guide. New England Medical Center, The Health Institute.
Waters, E. K., Doyle, Z., & Finlay, E. (2018). Spirituality/religiosity (SpR), leisure-time physical activity, and sedentary behaviors in students at a Catholic university. Journal of Religion & Health, 57(3), 869–882. https://doi.org/10.1007/s10943-017-0440-y
Webb, J. B., Siega-Riz, A. M., & Dole, N. (2012). Psychosocial determinants of adequacy of gestational weight gain. Obesity: A Research Journal, 17(2), 300-309. https://doi.org/10.1038/oby.2008.490
Williams, L. B., Franklin, B., Evans, M. B., Jackson, C., Hill, A., & Minor, M. (2016). Turn the beat around: A stroke prevention program for African-American churches. Public Health Nursing, 33(1), 11–20. https://doi.org/10.1111/phn.12234
World Health Organization. (2019). Physical activity. Global Strategy on Diet, Physical Activity and Health. https://www.who.int/dietphysicalactivity/pa/en/
*Address correspondence to:
Kimberly Feiler, Ph.D.
Health and Exercise Science Department
La Sierra University
Riverside, CA
Email: kfeiler@lasierra.edu
![]()
Journal of Kinesiology and Wellness © 2022 by Western Society for Kinesiology and Wellness is licensed under CC BY-NC-ND 4.0.