categories were created from frequently recurring categories. The third level is selective coding which connects the categories and subcategories to the core category. Subcategories were ideas or concepts that were related to a category. This level creates the theoretical framework of the study.
A group of peer researchers analyzed the text by independently reading through all the transcripts and following the steps outlined above. Throughout the entire data analysis, constant comparison was performed which compared all the words, sentences, paragraphs, codes, concepts, categories and literature. This method ensures that “emerging insights are grounded in all parts of the data and analysis” (Sparkes & Smith, 2014, p. 120).
Trustworthiness
To ensure the meaning of the participants’ interviews were accurate, member checking was performed with all participants. Participants were given a paragraph about the overall meaning of their interview. They were asked to confirm if the information was accurate and provide their thoughts on the subject. In addition, collaboration between research peers ensured that the interpretation of the data was not the reflection of a single person. These researchers read through all transcripts and their ideas on concepts and categories were discussed until consensus was reached.
FINDINGS AND DISCUSSION
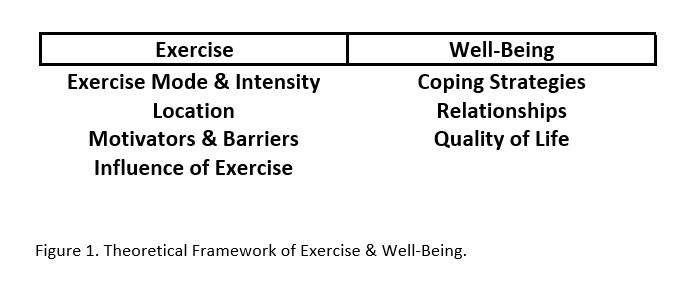
After all transcriptions were coded, two themes emerged: Exercise and Well-Being. Within these themes there were seven categories. Four categories for Exercise were labeled exercise mode and intensity, location, motivators and barriers, and influence of exercise. Three categories for Well-Being were labeled coping strategies, relationships, and quality of life. All categories had various concepts related to exercise which seemed to provide benefits for overall well-being. Figure 1 provides a visual representation of the theoretical framework based on the themes and categories. The theme names, Exercise and Well-Being encompass a spectrum of antecedents, behaviors, and outcomes surrounding exercise and PA. This study provides a broader picture of what leads participants to exercise, what types of activities they engage in for exercise, and the subsequent feelings, emotions, and behaviors resulting from their efforts to be physically active. In addition to identifying themes, guidelines for exercise programming for individuals with PTSD are proposed. To protect the anonymity of participants pseudonyms are used throughout the article.
Exercise
Exercise Mode and Intensity
All ten participants reported engaging in some form of exercise. Although inquiry included topics of both exercise and PA habits, most participants only discussed their exercise habits. Continuous and repetitive movement for cardiovascular exercise was most often reported, which included activities such as running and rowing on a machine.
With any form of exercise, including cardiovascular exercise, different intensities are often utilized for performance or health reasons. Exercise intensity may be an important factor to consider with this population. Higher intensity exercise can mimic symptoms of PTSD such as increased heart rate and sweating. The general population also tend to enjoy moderate intensity as opposed to vigorous intensity exercise (Lox, Ginis, & Petruzello, 2014.) Per the American College of Sport’s Medicine’s (ACSM) guidelines, adults should be engaging in at least 30 minutes of moderate intensity exercise on most days of the week for health, and all participants in the current study met those guidelines. This is important to note as it aids in the formation of exercise programming for individuals with PTSD and the ACSM’s guidelines can potentially be applied. Although participants were not asked why they participated in more moderate intensity exercises than vigorous, the explanations given above about exercise mimicking symptoms of PTSD may explain why more participants reported engaging in moderate intensity exercise.
Besides moderate intensity exercise, some participants also reported engaging in vigorous activity. Vigorous exercise affected John’s mood: “If I am pretty amped up, not necessarily in an anxious like vigilant mood, but more in an aggressive vigilant mood, weight training is not the best because it gets me more amped up.” However, research has demonstrated that the volume of vigorous exercise had an inverse relationship with posttraumatic stress symptoms while the volume of low to moderate intensity exercise did not (Harte, Vujanovic, & Potter, 2015). The researchers suggested this may be because repeated exposure to hyperarousal symptoms through vigorous intensity exercise may decrease their hyperarousal symptoms, however, further research is needed to make any conclusions. The intensity of the exercise may have some influence over participants’ symptoms, but other factors may contribute as well.
Location
Participants preferred performing exercise outside more often than inside, in settings such as a gym or at home. Natural environments have shown to be restorative which may be why participants preferred outside environments (Kaplan, 1995). Poulsen, Stigsdotter, Refshage (2015) reviewed 19 studies on nature-assisted therapy (activities done in the wild or in garden-type settings) and found that a majority provided a positive influence on people with PTSD and no negative influence. Wagenfield, Roy-Fisher, and Mitchell (2013) found similar results when exploring outdoor environments and concluded incorporating an outside environment with occupational therapy is ideal for veterans with PTSD. As discussed by Neil, environments such as a gym setting can be anxiety provoking:
There’s sometimes if a large group of individuals come in and I’m doing bench press and I get individuals on both sides of me, I’ll rerack everything and go find another bench to use so I don’t have individuals on both sides. It’s the anxiety. It starts to creep up when a lot of stuff is going on around me.
All strength training activities were done in a gym setting. John explained why he enjoys exercising outside: “Just out in nature like that it does something, it does something to the soul and to the mind. It's calming and relaxing.” This reflects the study done by Kaplan (1995) on how natural environments can be restorative. Taylor also mentioned nature when providing a reason for exercising outside. “I like you know, looking outside, seeing the leaves change” and she said that she likes to run near water because “it’s the most calming thing in the world” for her.
Motivators and Barriers
Participants also related some of their motivations and barriers to exercise. Most often, participants felt exercise provided stress relief for them both related and unrelated to their PTSD. In addition, participants explained the physical benefits exercise has on them. This finding is consistent with past research on the motivators for exercise and PA (Carless & Douglas, 2008; Erdner & Magnusson, 2012; Soundy, Kingstone, & Coffee, 2007). Neil related that exercise “relieves a lot of stress even if the stress isn’t PTSD related…it helps clear your mind and focus and just relieves a lot of undue stress…” Other motivators included a physical outlet and the physical benefits that come from exercising. Regarding her motivation for exercise, Margaret noted, “it’s strength to stay physically strong so that I can have a hopefully decent quality of life in my next set of golden years.”
Participants reported common barriers to exercise were related to their symptoms of PTSD, such as depression and fatigue, often due to lack of sleep and fear. John discussed his barriers to exercise related to his symptoms of PTSD:
So if I’ve had nightmares and I haven’t slept well or if I’ve had insomnia or something like that, that’ll definitely keep me from going…I’m so drained…more than just a physical drain from being tired but also a mental drain from the brain to process…Fear is debilitating…there are times that it’s just too much, it’s too much going on and I’m scared.
Barriers to exercise for Matt included depression and fear. “There are some days you just don’t want to get out of bed…Motivation for nothing. Scared of the outside world.” These findings were consistent with past research of individuals with mental disorders reporting that tiredness, feeling sad, and the illness itself were barriers to exercise (Carpiniello, Primavera, Pilu, Vaccargiu, & Pinna, 2013). Although no participant said crowded gyms or other environments were a barrier, it was mentioned as anxiety provoking.
Influence of Exercise
Exercise had a positive influence on all participants. Common positive influences were feeling good, happy, and in a better mood. When asked about what a good day entails, as defined by the participant, several included working out as a positive addition to their day. After he was first diagnosed with PTSD, exercise positively influenced Greg’s symptoms. “I would say [different exercises] positively influenced me. They reduced my symptoms in terms of the intensity, not necessarily the frequency.” Margaret talked about how exercise helps her both mentally and physically. “It helps me to be less anxious. I think it’s reduced stress…I feel stronger, I have a better self-image…it just, you know, makes me feel better about myself.” Increases in positive self-image due to exercise and PA are seen in other studies, including a study with individuals with mental disorders (Cullen & McCann, 2015). Furthermore, Anderson and Shivakumar (2013), discussed the anxiolytic effects of exercise both physically and psychologically. One of the psychological mechanisms through which exercise can influence anxiety is self-efficacy, given the relationship between self-efficacy and the ability to exert control over one’s life challenges (Anderson & Shivakumar, 2013). Although the exact mechanism through which exercise ameliorates anxiety is unclear, what is clear is the powerful influence of exercise on individuals with mental health concerns.
Well-Being
Coping Strategies
Besides exercise, participants also discussed other coping strategies they employed. Exploring other methods of coping in conjunction with exercise can help health professionals provide further guidance with the symptoms associated with PTSD. For example, participants used different tools and resources to cope with these symptoms including exercise, therapy, meditation, and social support. Several participants reported doing different forms of meditation, such as yoga and breathing exercises, and reported that it helped with their symptoms. This was consistent with previous research indicating that various forms of meditation may be an effective treatment for PTSD (Descilo et al., 2009; Lavey et al., 2005). Recently, Goldstein and colleagues (2018) created an integrative exercise program that included principles of mindfulness specifically tailored for veterans with PTSD. At the conclusion of the study, participants in the integrative exercise group showed reduced PTSD symptoms and increased perceptions of quality of life. Because of mindfulness-based principles, including paying attention to the moment, noticing mind wandering without judgement, and re-focusing on their current body state, individuals with PTSD may benefit from future integration of mindfulness and exercise.
Lack of social support, even with exercise, has been found as a barrier for individuals with PTSD and other mental illnesses (Yarborough, Stumbo, Yarborough, Young, & Green, 2016). Social support, in the form of friendships and spouses, was often mentioned by participants in this study, as a means of coping. Bridget explained that having friends who had experienced similar challenges was extremely helpful. She said, “That was probably the biggest help out of anything… it's hard if people haven't gone through the same experience. It's really hard to go through something like that and talk to [others who haven’t had the same experience] and have them somehow relate to it…because you just get exhausted with anything they say, which isn't fair to them, but you’re kind of like, eh you don't know.” In addition, several participants mentioned that support from family or friends was the impetus for seeking counseling or help prior to their diagnosis. In general, in this study, significant social relationships seemed to be a major source of support and coping.
One negative coping strategy mentioned by participants in this study was drinking. Substance use disorders are common amongst individuals with PTSD (Pietrzak, Goldstein Southwick, & Grant, 2011). In the current study, Greg is an example of what many participants described as a drinking problem. He said,
I picked up drinking. Um, the riskiest behaviors I had was alcohol and Vicodin, those two I mixed…I would just go home, turn on my computer, play video games and drink one big solid drink and then take a Vicodin and just chill out because nothing else was doing it.
It is not surprising that drinking was often mentioned in the present study as a coping mechanism, due to the high incidence rates among individuals with PTSD. Another participant, Matt said, “I didn't know what it was…I didn't know why I was acting the way I was and, um, stuff like that. I was getting real withdrawn, violent nightmares, and so I started drinking to cope with it.” Not surprisingly, previous investigations have examined alcohol addiction in trauma-exposed individuals. In fact, Medina et al. (2011) and Brown et al. (2009) have specifically examined the role of exercise as a means of reducing alcohol use. Thus, it would not be extreme to suggest that exercise and PA could be essential to a treatment plan for individuals with PTSD. Future research should continue to investigate coping strategies of individuals with PTSD.
These insights into what symptoms and challenges individuals with PTSD experience – whether exercise-related or not – are important in developing exercise and PA programs in order to target the obstacles faced.
Relationships
Relationships, especially marriages, were often mentioned as being negatively affected after the onset of symptoms in the present study, which can be detrimental to healthy behaviors, such as exercise, as mentioned above. The DSM-V states that interference with social relationships can be a symptom of PTSD. Research claims 5 to 10% of individuals with PTSD have lasting relationship problems (U.S. Department of Veterans Affairs, 2015). In addition, individuals with PTSD often feel disconnected from others and, because of some symptoms they are facing, cannot be intimate with others (U.S. Department of Veterans Affairs, 2015).
Some participants said because they could not cope with what was happening, their marriages ended. For example, Aaron said “during all the years where PTSD had its hold on me by the neck I didn't exercise. And my marriage dissolved…” Some participants even spoke about relationships with their friends and children being negatively affected as well. Isabel’s friendships were “impacted massively” and affected what she “could do in the evenings” because of having PTSD. Scott spoke about his relationship with his kids when they get hurt and expressed concern that he feels “a lack of caring.” He said he’d like to “hug them and tell them you know I’m so sorry, but I feel like I’m just holding them and I’m like you’re fine.” Aaron mentioned several relationships being affected by PTSD. “It ruined two marriages, it ruined my relationship with my kids, it ruined my relationship with friends…”
Quality of Life
It is not uncommon to find that individuals with PTSD report reduced quality of life, including poor physical functioning, more bodily pain, poor general health, less social activity, and compromised emotional and mental health (Wen, Shi, Li, Yuan, & Wang, 2012). In the current study, participants related their concerns of quality of life in relation to their symptoms of PTSD. Most commonly, participants said that PTSD has had a negative impact on their life. Because of the symptoms they experience, it poses daily challenges for them. Challenges included things such as feeling abnormal stress while driving, avoiding crowds, and coexisting with things that remind them of the event. It is important to explore the different challenges faced by individuals with PTSD as these may pose as barriers for exercise and PA. Symptoms are a daily challenge for Matt: All the symptoms I have they pretty much never end. Violent - I’m on meds now which keeps me in check a little bit, but real high and low moods. When I say high moods, I mean real violent acts…and then I’ll go into a deep depression where I don’t want to do anything, I don’t like being around individuals. I can do crowds just for a little bit and then I have to get away from it. The emotional numbing. I can shut off the world and not care about anything. Those are the tough ones, those are tough things to deal with when you push your family away. Every day is a challenge. I’ve gone from times where I want to commit suicide to ripping people’s heads off. It’s a real, real tough thing…I’ve got meds that help. I don’t have the ups and downs as much, I still do occasionally, but it’s more manageable now. So, if you want to say my quality of life is a little better now, I guess. There’s not a day that goes by that I don’t feel something, you know?
Injuries both related and unrelated to their PTSD were mentioned by many participants. However, all participants were still active. Although participants’ quality of life was affected, it seemed that they maintained active lives to help buffer the negatives associated with their diagnosis.
Exercise Programming
A secondary purpose of this study was to gain insights for exercise programming specific to individuals with PTSD. All participants were asked if they would participate in an exercise program specifically for individuals with PTSD. The majority responded that they would. Most would like to see an exercise program to be with a small group so they can interact with the others and get to know them and can talk about what is going on in their lives, including connecting with others about specifically dealing with PTSD. For example, John said,
In general, I would like to see kind of like a small group dynamic form, kind of like...Gosh almost sounds cliché, but I don't want to say a band of brothers but exactly that. Like just like 3-5 guys just you know working out together and, and discussing what's going on in their lives but not even just that but just life, just talking. A lot of times that helps just talking. Because you're not – you're focused on the conversation, you're not focused on other things. You know and then if there are issues, you know you can talk about it. You can talk about things with people and understand what you're going through and your goal is hopefully all the same and that's to utilize this exercise plan to help benefit the symptoms, you know, to help the symptoms so if everybody had the same goal and same wavelength, you know I think it could be, I mean, I think it could be huge.
This quote demonstrates several elements of exercise programming that may need special consideration for individuals with PTSD. Based on current literature and the responses of participants in this study, this section will provide insights into individual vs group exercise, exercise intensity, exercise mode, and location preference. Furthermore, we offer observations about the role of attention in exercise for those struggling with PTSD.
Individual or Group Exercise
As stated previously, participants mentioned they would like to engage in a small group exercise setting and with others who have been diagnosed with PTSD or people that they could relate to. The participants in the study do not like being in large crowds making a small group setting ideal for this population. Caddick, Smith, and Phoenix (2015) found after engaging combat veterans in a surfing program, participants stated they enjoyed the “social benefits it brought in terms of camaraderie with other veterans.” Matt expressed how he would be more likely to participate in exercise programs if it was with other veterans with PTSD. “A lot of guys with PTSD do better with other vets and individuals that understand because it’s individuals you fought with so for the most part the trust is there.” Greg said that he would want a social component and to “feel like you’re working towards a common goal.” Previous studies suggest that a social environment is often seen as a motivator for exercise and PA (Carless & Douglas, 2008; Cullen & McCann, 2015; Erdner & Magnusson, 2012). Isabel explained that having other people to go to exercise class with was especially helpful for her when struggling to leave the house. She said: I found that like it was almost like keeping an appointment, so like I had to go because I had already booked it and I found it easier to go. I didn't want to go anymore, but I found it easier because part of the self-discipline was taken away and then other people telling me I need to go is also helpful (laughs). People dragging me there physically – well not physically, but other people going as well…like, come on, let’s go together, tends to help.
The decision to participate in individual or group exercise is largely dependent upon the individual’s preference. Much of the current research on exercise treatments for PTSD is done in groups; little is done alone. Thus, future research should make this a point of emphasis. It may be that the preference for individual vs. group exercise is dependent on different factors. Individuals who find it difficult to be motivated to exercise seek group exercise settings. Individuals who are seeking reprieve from crowds and need the solace of exercise apart from others should feel encouraged to do so.
Exercise Intensity.
Based on the information provided when asked how often and how long the participants engaged in exercise every week, duration and frequency was formed. As stated previously, the ACSM recommends that healthy individuals should participate in moderate intensity exercise for 30 minutes most days of the week. This guideline is largely based on the effects of research on desired physiological outcomes and does not consider psychological outcomes when making these recommendations. However, individuals with PTSD are experiencing intense physiological and psychological symptoms. Thus, it would be careless to base guidelines for this population on a solely physiological recommendation for health.
Participants in the current study performed moderate-to-vigorous intensity exercise on most days of the week and reported that, generally, exercise helped with their symptoms. Previous research on recommended exercise intensity for PTSD sufferers is scarce. In one of the few studies to directly examine the relationship between exercise intensity and levels of PTSD symptoms, Harte, Vujanovic, and Potter (2015) found that, after controlling for gender and trauma types, there was an inverse relationship between vigorous exercise intensity and PTSD symptoms. In other words, individuals who exercised at a vigorous level experienced fewer symptoms of PTSD. However, Harte and colleagues caution that the results of their study should be interpreted with caution, as the equivalent effect size was small to medium. In the current study, participants reported exercising at a variety of intensities. Additionally, participants used PA – unstructured movement devoid of the aim for fitness improvements – to cope with their symptoms. This distinction is important as exercise and PA may serve different purposes for individuals with PTSD. When exercise is used as a means of coping with PTSD hyperarousal symptoms, it may be that vigorous intensity is key. Exercising at high intensity has been related inversely to using alcohol as a coping mechanism, which was mentioned previously as a detrimental coping mechanism among individuals with PTSD (Medina, Vijanovic, Smits, Irons, Zvolensky, & Bonn-Miller, 2011). Based on this information, we recommend that individuals with PTSD develop an exercise program that includes some vigorous intensity exercise along with enjoyable PA that is specific to the preference of the individuals (i.e., walking a dog, hiking, disc golf, yoga) as a regular part of their routines.
Exercise Mode
Participants were asked what modes of exercise they would most enjoy if they were to partake in an exercise program for PTSD. In regards to an exercise program for individuals with PTSD, participants reported wanting to engage in a variety of exercises. Continuous, repetitive, cardiovascular exercise, such as running, cycling, or swimming was common among the participants. The mechanisms behind the benefits of this type of activity may be that while participating individuals can “turn off” thought processes and deter attention from trauma-related thoughts. However, Isabel, one participant who loved to run for exercise, explained that exercising alone with time to think was sometimes challenging: I found that running helps, but I figured that was just because running was something I did to clear my mind anyway. So I don't know if it's just I naturally like running so running helps, but something like swimming or like just going to the gym and doing it by myself – basically things where my brain isn't occupied – can be detrimental. So if like I'm just swimming up and down the pool my brain has time to think and that doesn't necessarily feel any better because I end up like – I just keep thinking about the stuff that's not good.
It seems that individuals with PTSD will have to experiment with modes of exercise that provide them with the tools to cope with their psychological and physiological symptoms. Notably, several participants mentioned that yoga made them bored or gave them “too much time in their head.” These comments are insightful because previous PTSD exercise interventions in randomized controlled trials have been crafted around yoga (van der Kolk et al., 2014; Mitchell et al., 2014), which seems to be in opposition to the preferences of the majority of the participants in this study. In addition to aerobic exercise, many participants spoke of their involvement in resistance training or strength training of some kind. This could also be something that provides them with moderate-to-vigorous intensity exercise, in addition to occupying their thoughts with counting repetitions, keeping track of sets, or repeating motivational mantras. In contrast to the findings in this study, recent research seems to be focusing on mindfulness and more cognitive therapies for PTSD. It may be that participants in the current study were not well-trained in cognitive-based strategies to deal with their symptoms.
Types of PA were also mentioned as beneficial for dealing with PTSD. Activities such as disc golf, walking, spikeball, and bike rides with family were enjoyable and provided an outlet for participants. Thus, we recommend that individuals with symptoms of PTSD find a form of exercise that meets the needs of their attention – which was predominantly some form of dissociation or distraction from their thoughts during exercise, and preoccupying their thoughts with music or the challenge of the exercise itself. It may also be provident to engage in some form of enjoyable PA as a means of connecting with others or sparking feelings of enjoyment.
Location Preference
Overwhelmingly, participants in this study, preferred exercising outdoors. Scott, a military veteran, commented, “I'd rather walk 20 miles than, you know, spend a day in the gym,” and Isabel said, “I guess like, I just like the outdoors. I like the fresh air.” Finally, Bridget explained, “I just find it much more…restorative really to be outside and kind of more natural than to be inside working on a piece of equipment that doesn't go anywhere. That, to me, is just kind of odd.” Despite the general preference for outdoor exercise, a few participants did express their desire to use weights or participate in a class, which would necessitate being indoors. We recommend that preference be the guiding factor in where individuals with PTSD exercise, while keeping in mind that outdoor exercise activities may be beneficial in multiple ways, such a stress-reduction and enjoyment of nature.
The Role of Attention
When considering optimal modes of exercise and location preference for individuals suffering from PTSD, it may be a matter of attention and focus. Some studies have explored the importance of exercise for PTSD as guiding focus during exercise. It may be that during exercise, attentional focus shifts from thoughts that precipitate symptoms and provides an escape from distressing thoughts. Goldstein et al. (2018) examined the relationships between PTSD symptoms and focusing the mind during exercise. Participants had diagnosed PTSD and attended three 1-hour exercise sessions a week. A word or idea was presented at the beginning of the class and restated throughout the class. Prompts included words such as “breathe,” “focus,” “respect,” and “let go.” Compared to a control group, participants in the exercise group found reductions in their PTSD symptoms. Additionally, mindfulness, or focusing the mind on the sensations the body is feeling in the moment (while exercising), and not thinking about negative experiences, may lower hypervigilance (Mehling et al., 2017). When not exercising, participants found themselves thinking about things they did not want to think about. Scott mentioned, “…[when] you’re, like, driving you know you have time to focus on you know things you don’t want to think about, you know, and then long drives especially.” Exercise may provide a space for people living with PTSD to clear their minds and focus on the task they are performing instead, helping reduce symptoms. Taylor’s experience reflects this idea. He said, For mental state, it helps release…that excess energy that I build up and it keeps me mentally focused on what I need to do and it keeps me at a calm capacity and it actually makes me happier…Ya, I feel relaxed… just, you know, I feel a lot more mentally clear at the moment. It's a huge stress relief. That's a big part of it and I can just forget about bullshit. You know anything that's bothering me anything that constantly weighs on my mind, you know, it's not there so then that happens I like to go slow that's how I like to deal with it.
Taylor’s comments suggest that he appreciated exercise for the mental distraction it provided and the mental clarity he experienced afterwards.
Not all research supports the proposition that the benefit of exercise to individuals with PTSD is because it functions as a distraction. Fetzner and Asmundson (2015) performed a similar study as Goldstein and colleagues (2018) and found different results. Participants were in one of three groups: (1) performing exercise with prompts that were designed to fix their attention on “interoceptive effects of exercise,” (2) watching a nature documentary while exercising, and (3) a control group with no distractions or prompts. Although no differences were found between groups, Fetzner and Asmundson (2015) acknowledge that their sample was aerobically untrained and recommend that further research focus on the mechanisms of exercise to reduce symptoms of PTSD. It is also noteworthy that they were only using stationary cycling as their mode of exercise, which is a repetitious form of exercise that doesn’t demand high levels of attention. Because of the mixed research findings in this area, it is unclear exactly why exercise is a beneficial treatment to aid in the reduction of PTSD symptoms.
Despite researchers’ conclusions that exercise has been the cause of reduction in symptoms, we feel this may be a limited view because PTSD is a psychological and physiological condition (Anderson & Shivakumar, 2013). Other studies have used recreational therapy as an adjunctive treatment for PTSD where PA rather than structured exercise has been the primary mode of treatment. For example, a group of individuals with PTSD found that a fly-fishing excursion helped to alleviate their symptoms by creating a sense of peace and concentration on new skills (Bennett, Van Puymbroeck, Piatt, & Rydell, 2014). In another study, Hawkins, Townsend, and Garst (2016) propose a nature-based therapy program to help alleviate symptoms of PTSD, citing literature on attention restoration theory and the positive effects of being in nature. They suggest that outdoor education and wilderness therapy programs may be beneficial, not because of the exercise but because of the focused attention it requires. Aaron found exercising outside as beneficial for his symptoms, similar to previous studies: “That’s exactly that meditative zone that you might have been in and that’s what happens when I’m outside. I get to a meditative place. When I meditate, I find peace.” Further research is needed to conclude if exercise itself or the mind focused on what it is doing reduces the symptoms of PTSD.
CONCLUSION
The current study provided insight into the influence of exercise and PA on active individuals with PTSD. Participants engaged in mostly moderate-to-vigorous intensity repetitive exercise such as running and preferred to exercise outside. In addition, findings further supported previous studies that suggest exercise and PA yielded decreases in symptoms associated with PTSD. Based on the responses of participants, guidelines for exercise programming for this population was created. While this exploratory study was a first step, it can be used to discover what the best exercise and PA protocols are for individuals with PTSD.
There were several limitations to this study. In general, this study is meant to provide a glimpse into the exercise and PA experiences of individuals with PTSD. Because of the qualitative nature of the study, any generalizations must be viewed with the study design limitations in mind. Generalizations to larger populations must be made cautiously, yet during the interview process data saturation occurred, meaning that participants’ responses were repetitive signifying agreement. One limitation of the study is that only currently physically active individuals were interviewed. Future researchers should consider interviewing individuals with PTSD who were physically active in the past and inquire as to why they are no longer physically active, or vice versa. In addition, researchers could interview PTSD sufferers who are not active, but would like to be and what exercises and activities they believe would best suit them. Another limitation of the study was that it did not focus on a particular population such as combat veterans or women. Specific populations may give more insight into what protocols are best for certain groups, as there may be differences. A third limitation was that individuals self-reported having PTSD. Individuals may have not had a formal diagnosis of PTSD. However, even individuals who believe they have PTSD and experience similar symptoms still can give valuable information into their lifestyle. In future research, a licensed practitioner could formally diagnose participants.
Future researchers should seek out the lived experiences of individuals with PTSD rather than imposing outsider perspectives on what might be best for them. Additionally, researchers should further investigate differences in the source of trauma in PTSD populations to gather more information on what exercises and activities are most helpful. Additional information about fitness levels prior to PTSD diagnosis may also help to understand the exercise programming that is most helpful based on fitness levels. Furthermore, more intervention studies are needed to provide additional quantitative and qualitative information. The current study adds an insightful contribution to the growing, yet limited amount of research on PTSD and exercise. The research provides further support of exercise and PA as an effective coping mechanism and adjunct treatment for PTSD. Finally, this information provides a set of guidelines for exercise for individuals with PTSD.