DISCUSSION
The objective of this study was
to examine how the one-time use of PBWS could affect gait performance in older
adults with and without MS while dual-task walking. This study builds upon
prior work examining the benefits of PBWS (Chaparro et al., 2017; Danielsson
& Sunnerhagen, 2000; Field-Fote, 2001; Hesse et al., 1997; Miyai et al.,
2000; Ribeiro et al., 2013; Ullah et al., 2017; Visintin & Barbeau, 1989;
Visintin et al., 1998) and work examining how to improve dual-task gait
performance in older adults with MS (Monjezi et al., 2017; Peruzzi, 2016,
2017). To our knowledge, this was the first study to examine the effects of the
one-time use of PBWS on dual-task gait performance (as measured by gait
variability measures) in older adults with and without MS. Our findings
indicate that while older adults with MS exhibited greater decreases (i.e.,
improvements) in gait variability under PBWS when compared to NBWS, all
participants exhibited decreases in gait variability under PBWS. Together,
these results suggest that older adults with and without MS can benefit from
PBWS while dual-tasking as demonstrated by improvements in gait performance.
Thus, study findings highlight the importance for implementing PWBS for older
adults, but especially for older adults with MS.
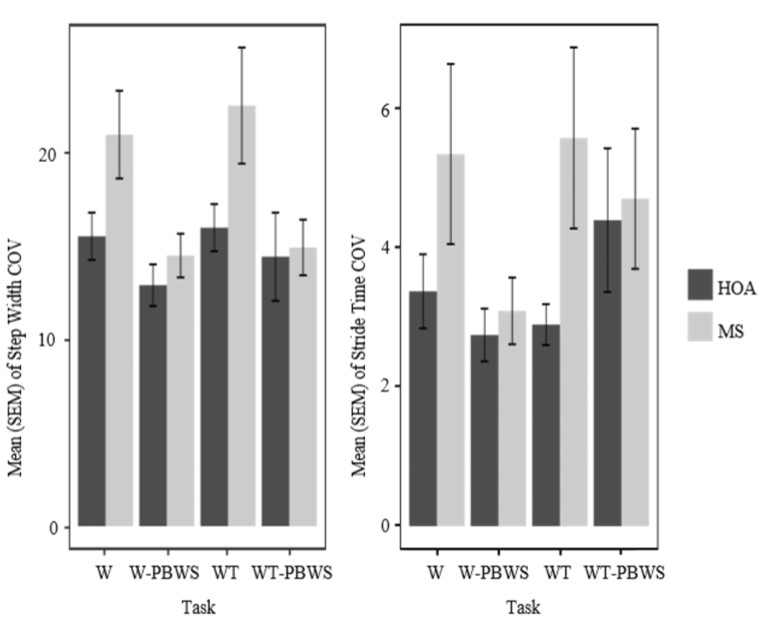
Consistent with
our hypothesis, while HOA did improve their gait performance (i.e., lower
COV-ST and COV-SW) under PBWS when compared to NBWS, the older adults with MS
exhibited greater improvements under PBWS. As can be seen in Figure 2 (both
COV-SW and COV-ST), while cohort differences exist under NBWS (for both single
and dual-task walking conditions), those differences disappear under PBWS
conditions. Thus, the study findings indicate that the older adults with MS
exhibited greater improvements in gait variability under PBWS which allowed
them to exhibit similar behavior as that of the healthy control. This is an
indication that older adults with MS benefitted more from PBWS conditions than
HOA. While research has established that individuals with MS experience lower
extremity muscle weakness which can negatively impact gait (Kalron et al.,
2011; Sandroff et al., 2013; Yahia et al., 2011), perhaps the use of PBWS in
this study assists with decreasing the physical load/demands for MS, overpowers
the effects of lower extremity weakness, and leads to gait improvements. On the
other hand, the larger COV-SW and COV-ST seen in MS under NBWS is similar to
findings in individuals with fibromyalgia (Heredia-Jimenez et al., 2016) and
mild cognitive impairment (Boripuntakul et al., 2014) who demonstrated higher
COV-SW when compared to a healthy control group, suggesting that symptoms of
pain or mild cognitive impairment in older adults with MS may contribute to
increased gait variability. Along with COV-SW, COV-ST has also been negatively
correlated with balance confidence (Nagano et al., 2014; Schinkel-Ivy et al.,
2016). Together, these results indicate that gait variability changes could be
sensitive to changes in physical and psychological function in older adults
with MS, and that the use of PBWS in older adults with MS can indeed serve as a
therapeutic tool for improving gait parameters while dual-tasking.
Furthermore, as
seen in Figure 2, all individuals (regardless of condition (i.e., MS or HOA))
exhibited lower COV-SW during PBWS conditions when compared to NBWS. Thus, the
use of PBWS acted as a tool to improve step width variability. This is
consistent with findings from Dragunas et al. (2016) where healthy young
individuals exhibited a decrease in COV-SW while walking with body weight
support. A larger COV-SW has been related to impaired balance (Nagano et al.,
2014) and thus able to identify fallers (Svoboda et al., 2017). Thus, the
smaller COV-SW under PBWS found in this study, indicates that individuals had
better balance under PBWS when compared to NBWS conditions. Together, these
results indicate that the one-time use of PBWS can exhibit positive effects on
gait symmetry variables in HOA and older adults with MS and thus improve the
ability to dual-task. It is important to note, that though this study did not
examine the effects of PBWS on the risk of falls, the gait behavior observed
under PBWS can be a reflection of a lower risk of falls in older adults with
MS.
Consistent with
the literature, when compared to single-task walking, all individuals
(regardless of group (i.e., MS or HOA)) exhibited a larger stride time
variability while dual-task walking (see Figure 2). Increases in stride time
variability has been exhibited while dual-tasking in healthy older adults
(Dubost et al., 2006) and older adults with dementia (Ijmker & Lamoth,
2012). This increase in variability during a dual-task has been found to be
attributed to a cognitive task requiring attention (Dubost et al., 2006) or
levels of executive function (Ijmker & Lamoth, 2012). Thus, the larger
stride time variability exhibited by the participants in the present study can
also be attributed to the cognitive task required to perform while walking or
level of executive function. However, given the focus of the paper on whether
gait performance in HOA and older adults with MS are influenced while
dual-tasking with an acute or single application of PBWS, the effects of PBWS
on measures of the cognitive performance or level of cognition were not
explicitly examined in this paper. Nonetheless, the increase in stride time
variability while dual-tasking can be explained by the shared attentional
capacity that leads to a decrease in gait automaticity (Nutt et al., 1993).
As expected,
when compared to the single-task walking under PBWS, COV-ST was higher for all
individuals (regardless of group (i.e., MS or HOA)) during dual-task walking
under NBWS (see Figure 2). Similarly, for individuals with MS, it has been
found that they exhibit greater gait variability measures while dual-tasking
when compared to single task walking and healthy controls (Hamilton et al.,
2009). This increase in COV-ST can be partly attributed to the addition of the
cognitive task which can decrease the amount of attention allocated towards
walking performance and thus cause an increase in COV-ST. Meanwhile, because
this study examined the effects of the one-time use of PBWS on gait
variability, perhaps these findings are due to the initial destabilizing effect
caused by PBWS. Thus, these findings require further exploration into the
possible effects of longer training periods using PBWS.
Contradictory to
our study findings, Kyvelidou et al. (2008) discovered that when compared to
younger adults and low levels of body weight support, older adults demonstrated
greater joint kinematic variability while walking with higher amounts of body
weight support. While they attribute their findings to the need of altering
proprioceptive information due to the decrease of gravitational stimulation
under PBWS, this study can attribute the opposing findings to the increase in
the ease of walking demands and decrease in the physical demands that are
required for walking under PBWS. While research has demonstrated improvements
in gait while dual-task walking after different dual-task training
interventions such as balance and cognitive dual-tasks (Monjezi et al., 2017)
and virtual reality treadmill training (Peruzzi, 2016, 2017), the population
examined were individuals with MS in middle adulthood (i.e., ages 30-40) and
the gait parameters measured included gait speed, stride length, and hip range
of motion. Thus, the present study findings contribute to the literature by
demonstrating improvements in gait variability in older adults with MS while
dual-task walking under a one-time use of PBWS.
Because this
study examined individuals with low levels of disability severity (median EDSS
score of 4.25) that had no significant mobility impairments present, these
findings cannot be generalized for individuals with MS with higher disability
levels with marked mobility impairments. Thus, future research should examine
the possible benefits of PBWS for individuals with higher disability severity
levels. Furthermore, given that the gait variability improvements observed
under PBWS were not tested for permanence, further work should examine the
long-term effects of PWBS on gait variability in older adults with MS. While
this study examined the effects on gait symmetry variables, future studies
should examine dynamic postural control variables to provide greater
sensitivity in identifying the benefits of PBWS on balance and gait. Lastly,
because the order of BWS conditions was fixed (i.e., NBWS conditions before
PBWS conditions), the authors acknowledge that the changes exhibited in the
present study can be a result from a practice effect. Thus, future research
should incorporate randomized BWS conditions into their methods.
CONCLUSION
This study was
the first to examine the effects of the one-time use of PBWS on the
dual-tasking gait variability of older adults with MS and compare it to age and
gender matched controls. Findings exhibited that PBWS can indeed improve gait
performance while dual-tasking which, though not examined in this study, can
reflect a decrease in the risk of falls. For a clinical population such as
older adults with MS, it was effectively demonstrated that PBWS can be
implemented for improving dual-tasking gait parameters. It has been discovered
that PBWS has the ability to improve gait parameters while dual-tasking in
older adults with MS. With further work examining the long-term benefits of
PBWS on gait variability, PBWS may be recommended by clinicians in order to
improve the dual-tasking ability and increase quality of life in HOA and older
adults with MS. In addition, the benefits observed after the one-time
use of PBWS can highlight the feasibility for researchers to incorporate
dual-tasking interventions under PBWS for these populations.
ACKNOWLEDGEMENT
We would like to thank the
participants in this study and the research staff in the Mobility and Fall
Prevention Research Laboratory for their assistance.
FUNDING
No funding declared to complete
this research.
REFERENCES
Allali,
G., Laidet, M., Assal, F., Armand, S., & Lalive, P. H. (2014). Walking
while talking in patients with multiple sclerosis: The impact of specific
cognitive loads. Neurophysiologie Clinique, 44(1), 87-93. doi:
10.1016/j.neucli.2013.10.136
Allali,
G., Laidet, M., Herrmann, F. R., Armand, S., Elsworth-Edelsten, C., Assal, F.,
& Lalive, P. H. (2016). Gait variability in multiple sclerosis: A better
falls predictor than EDSS in patients with low disability. Journal of Neural
Transmission, 123(4), 447-450. doi: 10.1007/s00702-016-1511-z
Amato,
M. P., Zipoli, V., & Portaccia, E. (2006) Multiple sclerosis-related
cognitive changes: A review of cross-sectional and longitudinal studies.
Journal of Neurological Sciences, 245(1-2), 41-46. doi:
10.1177/1747493018778713
Barela, A. M. F., Gama, G. L., Russo-Junior,
D.V., Celestino, M. L., & Barela, J. A. (2019). Gait alterations during
walking with partial body weight supported on a treadmill and over the ground. Scientific
Reports, 9(1), 8139. doi: 10.1038/s41598-019-44652-y
Boripuntakul, S., Lord, S. R., Brodie, M.
A., Smith, S. T., Methapatara, P., Wongpakaran, N., & Sungkarat, S. (2014).
Spatial variability during gait initiation while dual tasking is increased in
individuals with mild cognitive impairment. Journal of Nutrition, Health,
and Aging, 18(3), 307-312. doi: 10.1007/s12603-013-0390-3
Chaparro, G., Balto, J. M.,
Sandroff, B. M., Holtzer, R., Izzetoglu, M, Motl, R. W., &
Hernandez, M. E. (2017). Frontal brain activation changes due to dual-tasking
under partial body weight support conditions in older adults with multiple
sclerosis. Journal of Neuroengineering and Rehabilitation, 14(1), 65.
doi: 10.1186/s12984-017-0280-8.
D’Esposito, M., Onishi, K., Thompson, H.,
Robinson, K., Armstrong, C., & Murray, G. (1996). Working memory
impairments in multiple sclerosis: Evidence from a dual-task paradigm. Neuropsychology,
10(1), 51-56. http://dx.doi.org/10.1037/0894-4105.10.1.51
Danielsson, A., & Sunnerhagen, K. S.
(2000). Oxygen consumption during treadmill walking with and without body
weight support in patients with hemiparesis after stroke and in healthy
subjects. Archives of Physical Medicine and Rehabilitation, 81(7),
953-957. doi: 10.1053/apmr.2000.6283
de Oliveira, L. A. S., Martins, C. P.,
Horsczaruk, C. H. R., da Silva, D. C. L., Vasconcellos, L. F., Lopes, A. J.,
Mainenti, M. R. M., & Rodrigues, E. C. (2018). Partial body
weight-supported treadmill training in spinocerebellar ataxia. Rehabilitation
Research and Practice, 2018, 7172686. doi: 10.1155/2018/7172686
Dragunas, A. C., & Gordon, K. E.
(2016). Body weight support impacts lateral stability during treadmill walking.
Journal of Biomechanics, 49(13), 2662-2668. doi:
10.1016/j.jbiomech.2016.05.026
Dubost, V., Kressig, R. W., Gonthier, R.,
Herrmann, F. R., Aminian, K., Najafi, B., & Beauchet, O. (2006).
Relationships between dual-task related changes in stride velocity and stride
time variability in healthy older adults. Human Movement Science, 25(3),
372-382. doi: 10.1016/j.humov.2006.03.004
Faulkner, K. A., Redfern, M. S., Cauley, J.
A., Landsittel, D. P., Studenski, S. A., Rosano, C., Simonsick, E. M., Harris,
T. B., Shorr, R. I., Ayonayon, H. N., Newman, A. B., & Health, Aging, and
Body Composition Study. (2007) Multitasking: Association between poorer
performance and a history of recurrent falls. Journal of the American
Geriatrics Society, 55(4), 570-576. doi: 10.1111/j.1532-5415.2007.01147.x
Field-Fote, E. C. (2001).
Combined use of body weight support, functional electric stimulation, and
treadmill training to improve walking ability in individuals with chronic
incomplete spinal cord injury. Archives of Physical Medicine and
Rehabilitation, 82(6), 818–824. doi: 10.1053/apmr.2001.23752
Finlayson, M. (2004). Concerns about the
future among older adults with multiple sclerosis. American Journal of
Occupational Therapy, 58(1), 54-63. doi: 10.5014/ajot.58.1.54
Finlayson, M. L., Peterson, E. W., &
Cho, C. C. (2006). Risk factors for falling among people aged 45 to 90 years
with multiple sclerosis. Archives of Physical Medicine and Rehabilitation,
87(9), 1274-1279. doi: 10.1016/j.apmr.2006.06.002
Hamilton, F., Rochester, L.,
Paul, L., Rafferty, D., O’Leary, C. P., & Evans, J. J. (2009). Walking and
talking: an investigation of cognitive-motor dual tasking in multiple
sclerosis. Multiple Sclerosis, 15(10), 1215-1227. doi:
10.1177/1352458509106712
Heredia-Jimenez, J., Orantes-Gonzalez, E.,
& Soto-Hermoso, V. M. (2016) Variability of gait, bilateral coordination,
and asymmetry in women with fibromyalgia. Gait & Posture, 45, 41-44.
doi: 10.1016/j.gaitpost.2016.01.008
Hesse, S., Helm, B., Krajnik,
J., Gregoric, M., &
Mauritz, K. H. (1997).
Treadmill training with partial body weight support: Influence of body weight
release on the gait of hemiparetic patients. Neurorehabilitation and Neural
Repair, 11, 15-20. doi.org/10.1177/154596839701100103
Ijmker, T., & Lamoth, C. J. (2012).
Gait and cognition: The relationship between gait stability and variability
with executive function in persons with and without dementia. Gait
&Posture, 35(1), 126-130. doi: 10.1016/j.gaitpost.2011.08.022
Kalron, A. (2017). Association between gait
variability, falls and mobility in people with multiple sclerosis: A specific
observation on the EDSS 4.0-4.5 level. NeuroRehabilitation, 40(4),
579-585. doi: 10.3233/NRE-171445
Kalron, A., Achiron, A., & Dvir, Z.
(2011). Muscular and gait abnormalities in persons with early onset multiple
sclerosis. Journal of Neurologic Physical Therapy, 35(4), 164-169. doi:
10.1097/NPT.0b013e31823801f4
Kurtzke, J. F. (1983). Rating neurologic
impairment in multiple sclerosis: An expanded disability status scale (EDSS). Neurology,
33(11), 1444-1452. doi: 10.1212/wnl.33.11.1444
Kyvelidou, A., Kurz, M. J., Ehlers, J.L.,
& Stergiou, N.
(2008). Aging and partial body weight
support affects gait variability. Journal of Neuroengineering and
Rehabilitation, 5(22), doi: 10.1186/1743-0003-5-22
Learmonth, Y. C., Sandroff,
B. M., Pilutti, L. A., Klaren, R. E., Ensari, I., Riskin, B. J., Holtzer R.,
& Motl, R. W. (2014). Cognitive motor interference during walking in
multiple sclerosis using an alternate-letter alphabet task. Archives
of Physical Medicine and Rehabilitation, 95(8), 1498-1503. doi:
10.1016/j.apmr.2014.03.007
Leone, C., Patti, F., & Feys, P.
(2015). Measuring the cost of cognitive-motor dual tasking during walking in
multiple sclerosis. Multiple Sclerosis, 21(2), 123–131. doi:
10.1177/1352458514547408
Lindquist, A. R., Prado, C. L., Barros, R.
M., Mattioli, R., da Costa, P. H., & Salvini, T. F. (2007). Gait training
combining partial body-weight support, a treadmill, and functional electrical
stimulation: Effects on poststroke gait. Physical Therapy, 87,
1144-1154. doi: 10.2522/ptj.20050384
Lundin-Olsson, L., Nyberg, L., &
Gustafson, Y. (1997). “Stops walking when talking” as a predictor of falls in
elderly people. Lancet, 349(9052), 617. doi:
10.1016/S0140-6736(97)24009-2
Luo, Y., Shen, W., Jiang, Z., & Sha, J.
(2016). Treadmill training with partial body-weight support after anterior
cruciate ligament reconstruction: A randomized controlled trial. Journal of
Physical Therapy Science, 28(12), 3325-3329. doi: 10.1589/jpts.28.3325
Martin, C. L., Phillips, B. A., Kilpatrick,
T. J., Butzkueven, H., Tubridy, N., McDonald, E., & Galea, M. P. (2006).
Gait and balance impairment in early multiple sclerosis in the absence of
clinical disability. Multiple Sclerosis, 12(5), 620-628. doi:
10.1177/1352458506070658
Miyai, I., Fujimoto, Y.,
Ueda, Y., Yamamoto, H., Nozaki, S., Saito, T., & Kang, J. (2000). Treadmill
training with body weight support: Its effect on Parkinson’s disease. Archives
of Physical Medicine and Rehabilitation, 81(7), 849–852. doi:
10.1053/apmr.2000.4439
Monjezi, S., Negahban, H., Tajali, S.,
Yadollahpour, N., & Majdinasab, N. (2017). Effects of dual-task balance
training on postural performance in patients with multiple sclerosis. Clinical
Rehabilitation, 31(2), 234-241. doi: 10.1177/0269215516639735
Montero-Odasso, M., Muir, S. W., &
Speechley, M. (2012). Dual task complexity affects gait in people with mild
cognitive impairment: The interplay between gait variability, dual tasking, and
risk of falls. Archives of Physical Medicine and Rehabilitation, 93(2),
293-299. doi: 10.1016/j.apmr.2011.08.026
Moon, Y., Wadja, D. A., Motl, R. W., &
Sosnoff, J. J. (2015). Stride-time variability and fall risk in persons with
multiple sclerosis. Multiple Sclerosis International, 2015, 964790. doi:
10.1155/2015/964790
Nagano, H., James, L., Sparrow, W. A.,
& Begg, R. K. (2014). Effects of walking-induced fatigue on gait function
and tripping risks in older adults. Journal of Neuroengineering and
Rehabilitation, 11, 155. doi: 10.1186/1743-0003-11-155
Nutt, J. G., Marsden, C. D., &
Thompson, P. D. (1993). Human walking and higher-level gait disorders,
particularly in the elderly. Neurology, 43(2), 268-279. doi:
10.1212/wnl.43.2.268
Peruzzi, A., Cereatti, A., Della Croce, U.,
& Mirelman, A. (2016). Effects of a virtual reality treadmill training on
gait of subjects with multiple sclerosis: A pilot study. Multiple Sclerosis
and Related Disorders, 5, 91-96. doi: 10.1016/j.msard.2015.11.002
Peruzzi, A., Zarbo, I. R., Cereatti, A.,
Della Croce, U., & Mirelman, A. (2017). An innovative training program
based on virtual reality and treadmill: effects on gait of persons with
multiple sclerosis. Disability and Rehabilitation, 39(15), 1557-1563.
doi: 10.1080/09638288.2016.1224935
Ribeiro, T., Britto, H., Oliveira, D.,
Silva, E., Galvao, E., & Lindquist, A. (2013). Effects of treadmill
training with partial body weight support and the proprioceptive neuromuscular
facilitation method on hemiparetic gait: A randomized controlled study. European
Journal of Physical Rehabilitation Medicine, 49(4), 451-461.
Sanai, S. A., Saini, V., Benedict, R. H.,
Zivadinov, R., Teter, B. E., Ramanathan, M., & Weinstock-Guttman, B.
(2016). Aging and multiple sclerosis. Multiple Sclerosis, 22(6),
717-725. doi: 10.1177/1352458516634871
Sandroff, B. M., Sosnoff, J. J., &
Motl, R. W. (2013). Physical fitness, walking performance, and gait in multiple
sclerosis. Journal of Neurological Sciences, 328(1-2), 70-76. doi:
10.1016/j.jns.2013.02.021
Schinkel-Ivy, A., Inness, E. L., &
Mansfield, A. (2016). Relationships between fear of falling, balance
confidence, and control of balance, gait, and reactive stepping in individuals
with sub-acute stroke. Gait & Posture, 43, 154-159. doi:
10.1016/j.gaitpost.2015.09.015
Socie, M. J., Motl, R. W., Pula, J. H.,
Sandroff, B. M., & Sosnoff, J. J. (2013). Gait variability and disability
in multiple sclerosis. Gait & Posture, 38(1), 51-55. doi:
10.1016/j.gaitpost.2012.10.012
Sosnoff, J. J., Boes, M. K.,
Sandroff, B. M., Socie, M. J., Pula, J. H., & Motl, R. W. (2011). Walking
and thinking in persons with multiple sclerosis who vary in disability. Archives
of Physical Medicine and Rehabilitation, 92(12), 2028-2033. doi:
10.1016/j.apmr.2011.07.004
Sosnoff, J. J., Sandroff, B. M., &
Motl, R. W. (2012). Quantifying gait abnormalities in persons with multiple
sclerosis with minimal disability. Gait & Posture, 36(1), 154-156.
doi: 10.1016/j.gaitpost.2011.11.027
Springer, S., Giladi, N., Peretz, C.,
Yogev, G., Simon, E. S., & Hausdorff, J. M. (2006). Dual-tasking effects on
gait variability: The role of aging, falls, and executive function. Movement
Disorders, 21(7), 950-957. doi: 10.1002/mds.20848
Svoboda, Z., Bizovska, L., Janura, M.,
Kubonova, E., Janurova, K., & Vuillerme, N. (2017). Variability of spatial
temporal gait parameters and center of pressure displacements during gait in elderly
fallers and nonfallers: A 6-month prospective study. PloS One, 12(2),
e0171997. doi: 10.1371/journal.pone.0171997
Ullah, M. A., Shafi, H.,
Khan, G. A., Malik, A. N., & Amjad, I. (2017). The effects of gait training
with body weight support (BWS) with no body weight support (no-BWS) in stroke
patients. Journal of the Pakistan Medical Association, 67(7), 1094-1096.
Verghese, J., Buschke, H., Viola, L., Katz,
M., Hall, C., Kuslansky, G., & Lipton, R. (2002). Validity of divided
attention tasks in predicting falls in older individuals: A preliminary study. Journal
of the American Geriatrics Society, 50, 1572-1576. doi:
10.1046/j.1532-5415.2002.50415.x
Visintin, M., & Barbeau, H. (1989). The
effects of body weight support on the locomotor pattern of spastic paretic
patients. Canadian Journal of Neurological Sciences, 16(3), 315-325.
doi: 10.1017/s0317167100029152
Visintin, M., Barbeau, H.,
Korner-Bitensky, N., & Mayo, N. (1998). A new approach to retrain gait in
stroke patients through body weight support and treadmill stimulation. Stroke,
29(6), 1122-1128. doi: 10.1161/01.str.29.6.1122
Wajda, D. A., & Sosnoff, J. J. (2015).
Cognitive-motor interference in multiple sclerosis: A systematic review of
evidence, correlates, and consequences. BioMed Research Institute, 2015,
720856. doi: 10.1155/2015/720856
Welsh, K. A., Breitner, J. C. S., &
Magruder-Habib, K. M. (1993). Detection of dementia in the elderly using
telephone screening of cognitive status. Neuropsychiatry, Neuropsychology
and Behavioral Neurology, 6(2): 103-110.
Yahia, A., Ghroubi, S., Mhiri, C., &
Elleuch, M. H. (2011). Relationship between muscular strength, gait and
postural parameters in multiple sclerosis. Annals of Physical Rehabilitation
Medicine, 54(3), 144-155. doi: 10.1016/j.rehab.2011.02.004
![]() test was used
to examine gender differences between the groups. To test our primary
hypothesis, a linear mixed-model was used to examine differences between cohort
(MS and HOA), task (W and WT), and body weight support (BWS) (NBWS and PBWS)
for COV-SW and COV-ST, separately. Random intercepts were included: by-subject,
by-BWS, and by-task. The necessary tests were run to test for normality and
outliers. The rankit
test was used
to examine gender differences between the groups. To test our primary
hypothesis, a linear mixed-model was used to examine differences between cohort
(MS and HOA), task (W and WT), and body weight support (BWS) (NBWS and PBWS)
for COV-SW and COV-ST, separately. Random intercepts were included: by-subject,
by-BWS, and by-task. The necessary tests were run to test for normality and
outliers. The rankit